
A mathematical model developed by a researcher distinguishes small, intermediate, and large-sized droplets, allowing for easy determination of a droplet’s maximum range using simple formulas.
A mathematical model of droplet migration may have important implications for understanding the spread of airborne diseases, such as COVID-19.
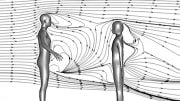
The World Health Organization has warned that aerosol transmission of COVID-19 is being underestimated. If aerosol spread is confirmed to be significant, as suspected, we will need to reconsider guidelines on social distancing, ventilation systems, and shared spaces.
A group of researchers from Heriot-Watt University and the University of Edinburgh in the U.K. believes a better understanding of different droplet behaviors and their different dispersion mechanisms based on droplet size is also needed.
In the journal Physics of Fluids, from AIP Publishing, the group presents a mathematical model that clearly demarcates small-, intermediate- and large-sized droplets. Simple formulas can be used to determine a droplet’s maximum range.
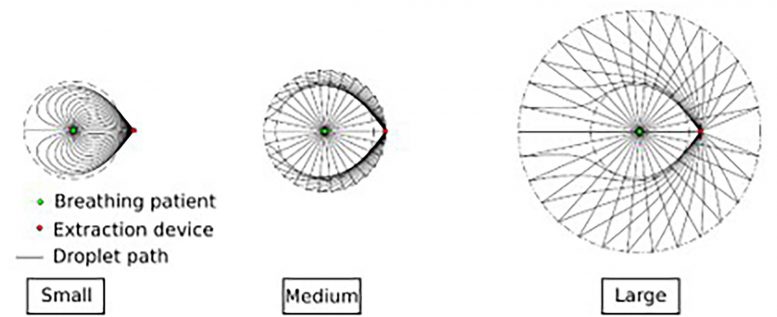
Droplet paths from patient to extraction device: small, medium, and large droplets. Credit: Cathal Cummins
This has important implications for understanding the spread of airborne diseases, such as COVID-19, because their dispersion tests revealed the absence of intermediate-sized droplets, as expected.
“The flow physics of someone coughing is complex, involving turbulent jets and droplet evaporation,” said Cathal Cummins, of Heriot-Watt University. “And the rise of COVID-19 has revealed the gaps in our knowledge of the physics of transmission and mitigation strategies.”
One such gap in the physics is a clear, simple description of where individual droplets go when ejected.
“We wanted to develop a mathematical model of someone breathing that could be explored analytically to examine the dominant physics at play,” Cummins said.
As a person breathes, they emit droplets of various sizes that don’t necessarily follow the airflow faithfully.
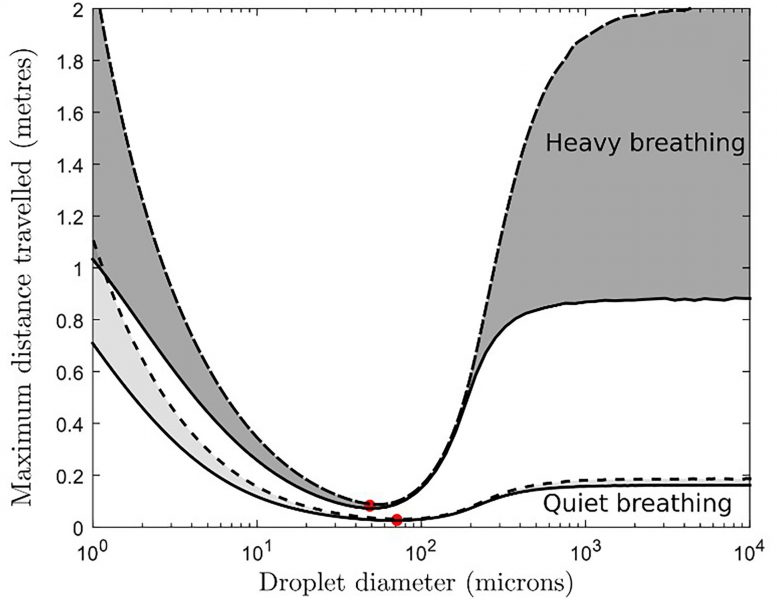
Maximum horizontal distance covered by exhaled water droplets for various droplet diameters: heavy vs. quiet breathing. The red dot indicates the global minimum in distance covered. In this case, the minimum is attained for droplets of diameters between 50 and 80 microns. Credit: Cathal Cummins
“We represent breathing as a point source of both air and droplets and include a point sink to model the effect of extraction of air and droplets,” Cummins said. “To take their size and density differences into account, we use the Maxey-Riley equation, which describes the motion of a small but finite-sized rigid sphere through a fluid.”
This work gives researchers a general framework to understand the droplet dispersion. The model simplicity demonstrates that bimodality could actually be a property of the droplets themselves, and the group provides formulas to predict when such droplets will have short ranges.
“Our study shows there isn’t a linear relation between droplet size and displacement — with both small and large droplets traveling further than medium-sized ones,” said Felicity Mehendale, co-author and academic surgeon at the University of Edinburgh. “We can’t afford to be complacent about small droplets. PPE is an effective barrier to large droplets but may be less effective for small ones.”
As a solution, Mehendale came up with the idea of creating an aerosol extractor device. The team is working on plans to manufacture the aerosol extractor to keep clinicians safe during a wide range of aerosol-generating procedures routinely performed in medicine and dentistry. Extraction units placed near the droplet sources can effectively trap droplets, if their diameters fall below that of a human hair.
“This has important implications for the COVID-19 pandemic,” said Cummins. “Larger droplets would be easily captured by PPE, such as masks and face shields. But smaller droplets may penetrate some forms of PPE, so an extractor could help reduce the weakness in our current defense against COVID-19 and future pandemics.”
Mehendale said a better understanding of the droplet behavior will help “inform the safety guidelines for aerosol-generating procedures, and it will be relevant during the current and future pandemics, as well as for other infectious diseases. This mathematical model may also serve as the basis of modeling the impact on droplet dispersion of ventilation systems existing within a range of clinical spaces.”
Reference: “The dispersion of spherical droplets in source-sink flows and their relevance to the COVID-19 pandemic” is by C.P. Cummins, O.J. Ajayi, F.V. Mehendale, R. Gabl and I.M. Viola, 4 August 2020, Physics of Fluids.
DOI: 10.1063/5.0021427





This model does not seem to take into account the formation and transport of “droplet nuclei” by evporation, as studied by Wells and Riley in the 1930’s and may give the false impression that particles smaller than, say, 20 microns, are only capable of travelling some 20 or 30 cm, whereas their reduced terminal fall velocity is reduced to the point at which air currents can enable them to float for many tens of metres from their source.