
A 4-month study on people with non-alcoholic fatty liver disease (NAFLD) has shown that daily intake of resistant starch can modify gut bacteria and significantly reduce liver triglycerides and enzymes tied to liver damage. The study also revealed that these positive effects are independent of body weight changes.
Resistant starch, a type of indigestible fiber that undergoes fermentation in the large intestine, has previously demonstrated promising effects on metabolism in studies conducted on animals. Now, a four-month-long randomized controlled study involving individuals with non-alcoholic fatty liver disease (NAFLD) revealed that consuming resistant starch daily can positively influence gut microbiota dynamics and decrease levels of liver triglycerides and enzymes that are typically linked to liver damage and inflammation.
The findings of this study were recently published in the journal Cell Metabolism.
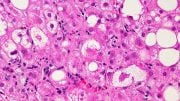
NAFLD, caused by a buildup of fat in the liver, affects about 30% of the population worldwide. It can lead to severe liver diseases and contribute to other conditions, such as type 2 diabetes and cardiovascular disease. Currently, there is no approved medicine available to treat NAFLD. Doctors usually recommend dietary changes and exercise to alleviate the conditions.
“We think it would be very meaningful if we can find an effective approach, maybe through identifying new therapeutic targets, to manage NAFLD,” says Huating Li, the paper’s co-corresponding author at Shanghai Sixth People’s Hospital.
Previous research has suggested that NAFLD is associated with perturbed gut microbiota. For example, people with early-stage NAFLD already have an altered gut bacteria profile. So, Li and her team wanted to investigate if resistant starch—a type of fiber known to encourage the growth of beneficial gut bacteria—can help treat NAFLD.
The team recruited 200 NAFLD patients and provided them with a balanced dietary plan designed by a nutritionist. Among them, 100 patients also received a resistant starch powder derived from maize while the other 100 received calorie-matched non-resistant corn starch as a control. They were instructed to drink 20 grams of the starch mixed with 300 mL water (1 ¼ cups) before meals twice a day for 4 months.
After the 4-month experiment, participants who received the resistant starch treatment had nearly 40% lower liver triglyceride levels compared to patients in the control group. In addition, patients who had the resistant starch treatment also saw reductions in liver enzymes and inflammatory factors associated with NAFLD. Importantly, these benefits were still apparent even when statistically adjusted for weight loss.
“Our study shows resistant starch’s impact in improving patients’ liver conditions is independent of body weight changes,” says Yueqiong Ni, the paper’s co-first author at Shanghai Sixth People’s Hospital and Leibniz Institute for Natural Product Research and Infection Biology – Hans-Knöll-Institute (HKI) in Germany.
By analyzing patients’ fecal samples, the team found the resistant starch group had a different microbiota composition and functionality compared with the control. In particular, the treatment-group patients had a lower level of Bacteroides stercoris, a key bacterial species that can affect fat metabolism in the liver through its metabolites. The reduction in B. stercoris is strongly linked to the decrease in liver triglyceride content, liver enzymes, and metabolites observed.
When the team transplanted fecal microbiota from resistant starch-treatment patients to mice fed with a high-fat high-cholesterol diet, the mice saw a significant reduction in liver weight and liver triglyceride levels and improved liver tissue grading compared with mice that received microbiota from the control group.
“We are able to identify a new intervention for NAFLD, and the approach is effective, affordable, and sustainable. Compared with strenuous exercise or weight loss treatment, adding resistant starch to a normal and balanced diet is much easier for people to follow through,” Li says.
Reference: “Resistant starch decreases intrahepatic triglycerides in patients with NAFLD via gut microbiome alterations” by Yueqiong Ni, Lingling Qian, Sara Leal Siliceo, Xiaoxue Long, Emmanouil Nychas, Yan Liu, Marsena Jasiel Ismaiah, Howell Leung, Lei Zhang, Qiongmei Gao, Qian Wu, Ying Zhang, Xi Jia, Shuangbo Liu, Rui Yuan, Lina Zhou, Xiaolin Wang, Qi Li, Yueliang Zhao, Hani El-Nezami and Weiping Jia, 5 September 2023, Cell Metabolism.
DOI: 10.1016/j.cmet.2023.08.002
The study was funded by the National Natural Science Foundation of China (NSFC), Shanghai Municipal Key Clinical Specialty, Shanghai Research Center for Endocrine and Metabolic Diseases, the National Key Research and Development Program of China, the Marie Sklodowska-Curie Actions (MSCA) and Innovative Training Networks, the National Key Research and Development Program of China (2022YFA1004804), Shanghai Jiao Tong University School of Medicine, the Dalian Institute of Chemical Physics, Chinese Academy of Sciences, and the Key Foundation.








Where do you find resistant starch? Is it natural or created in a lab?
Is it possible to get this supplement?
Is it possible to get this supplement?