A study using human cerebral organoids found that chronic wasting disease (CWD) is unlikely to transmit from deer, elk, and moose to humans, reinforcing the strong species barrier observed in earlier research.
Research on cerebral organoids provides strong evidence for a significant species barrier.
A recent study employing a human cerebral organoid model to investigate prion diseases indicates a significant species barrier that blocks the transmission of chronic wasting disease (CWD) from cervids—such as deer, elk, and moose—to humans. Conducted by scientists at the National Institutes of Health (NIH) and published in Emerging Infectious Diseases, the study’s results align with many years of similar research conducted at the NIH’s National Institute of Allergy and Infectious Diseases (NIAID).
Prion diseases are degenerative diseases found in some mammals. These diseases primarily involve deterioration of the brain but also can affect the eyes and other organs. Disease and death occur when abnormal proteins fold, clump together, recruit other prion proteins to do the same, and eventually destroy the central nervous system. Currently, there are no preventive or therapeutic treatments for prion diseases.

A researcher holds a flask containing human cerebral organoids similar to those used in the CWD study. Credit: NIAID
CWD is a type of prion disease found in cervids, which are popular game animals. While CWD has never been found in people, a question about its transmission potential has lingered for decades: Can people who eat meat from CWD-infected cervids develop prion disease? The question is important because during the mid-1980s and mid-1990s a different prion disease – bovine spongiform encephalopathy (BSE), or mad cow disease – emerged in cattle in the United Kingdom (U.K.) and cases also were detected in cattle in other countries, including the United States.
Over the next decade, 178 people in the U.K. who were thought to have eaten BSE-infected beef developed a new form of a human prion disease, variant Creutzfeldt-Jakob Disease, and died. Researchers later determined that the disease had spread among cattle through feed tainted with infectious prion protein. The disease transmission path from feed to cattle to people terrified U.K. residents and put the world on alert for other prion diseases transmitted from animals to people, including CWD. CWD is the most transmissible of the prion disease family, showing highly efficient transmission between cervids.
Advances in Prion Disease Research
Historically, scientists have used mice, hamsters, squirrel monkeys, and cynomolgus macaques to mimic prion diseases in people, sometimes monitoring animals for signs of CWD for more than a decade. In 2019, NIAID scientists at Rocky Mountain Laboratories in Hamilton, Montana, developed a human cerebral organoid model of Creutzfeldt-Jakob Disease to evaluate potential treatments and to study specific human prion diseases.
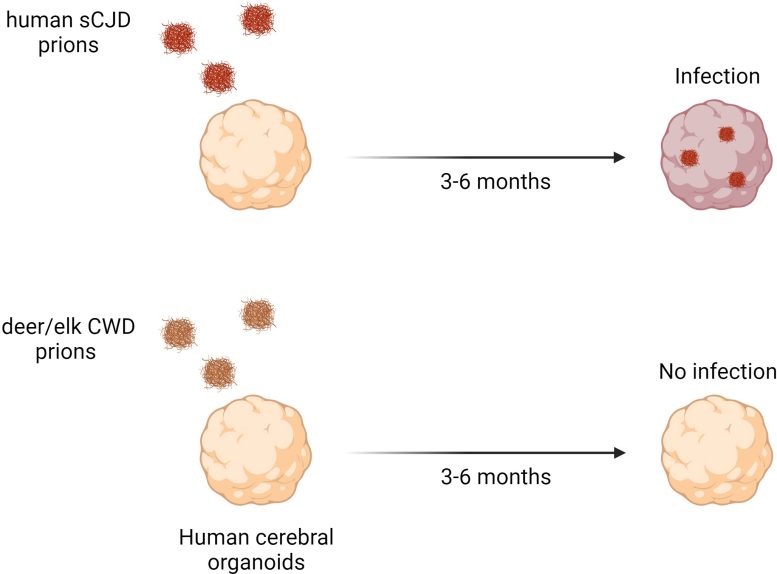
The top frames show the validated study model, where CJD brain matter (in red) infected the organoid. The bottom frames show the uninfected organoid after exposure to infectious CWD matter. Credit: NIAID
Human cerebral organoids are small spheres of human brain cells ranging in size from a poppy seed to a pea. Scientists grow organoids in dishes from human skin cells. The organization, structure, and electrical signaling of cerebral organoids are similar to brain tissue. They are currently the closest available laboratory model to the human brain. Because organoids can survive in a controlled environment for months, scientists use them to study nervous system diseases over time. Cerebral organoids have been used as models to study other diseases, such as Zika virus infection, Alzheimer’s disease, and Down syndrome.
In the new CWD study, the bulk of which was done in 2022 and 2023, the research team validated the study model by successfully infecting human cerebral organoids with human CJD prions (positive control). Then, using the same laboratory conditions, they directly exposed healthy human cerebral organoids for seven days with high concentrations of CWD prions from white-tailed deer, mule deer, elk, and normal brain matter (negative control). The researchers then observed the organoids for up to six months, and none became infected with CWD.
This indicates that even following direct exposure of human central nervous system tissues to CWD prions there is a substantial resistance or barrier to the propagation of infection, according to researchers. The authors acknowledge the limitations of their research, including the possibility that a small number of people may have genetic susceptibility that was not accounted for, and that the emergence of new strains with a lesser barrier to infection remains possible. They are optimistic that the inference of these current data is that humans are extremely unlikely to contract a prion disease because of inadvertently eating CWD-infected cervid meat.
Reference: “Lack of Transmission of Chronic Wasting Disease Prions to Human Cerebral Organoids” by Bradley R. Groveman, Katie Williams, Brent Race, Simote Foliaki, Tina Thomas, Andrew G. Hughson, Ryan O. Walters, Wenquan Zou and Cathryn L. Haigh, June 2024, Emerging Infectious Diseases.
DOI: 10.3201/eid3006.231568
The research was funded by the National Institute of Allergy and Infectious Diseases.








Be the first to comment on "NIH Study Confirms: Humans Unlikely To Catch Deer Prion Disease"