New research reveals that individuals at higher risk of developing psychosis exhibit brain irregularities even before the onset of schizophrenia, providing a potential marker for the disease and explaining its typical manifestation in young adulthood.
New research from Yale University reveals that even before the onset of schizophrenia, irregularities in key brain areas are already present in individuals at higher risk of developing psychosis.
The findings identify a potential marker for the debilitating disease that afflicts 1% of the world’s population and suggest at least a partial explanation for why schizophrenia most typically manifests itself in young adulthood.
The new study, published online August 12 in the journal JAMA Psychiatry, builds on work at Yale that shows schizophrenia is associated with marked alterations in connections between the thalamus, a major relay system in the brain, and the frontal cortex, which is involved in higher-level cognitive functions.
“Up until this study, we did not know whether this pattern was a result of the disease or a potential byproduct of medication or some other factor,” said Alan Anticevic, assistant professor of psychiatry and lead author of the paper. “We show these same abnormalities already exist in people who are at higher risk for developing psychosis.”
Schizophrenia usually develops late in adolescence or early adulthood but is often proceeded by some early warning signs such as mild suspicion, a perception that outside stimuli carry a special personal significance, or hearing a voice calling the individual’s name, said Tyrone Cannon, professor of psychology and senior author of the study.
In chronic schizophrenia, especially if untreated, these symptoms worsen and can become debilitating. It has been unclear exactly what brain mechanisms are responsible for its onset.
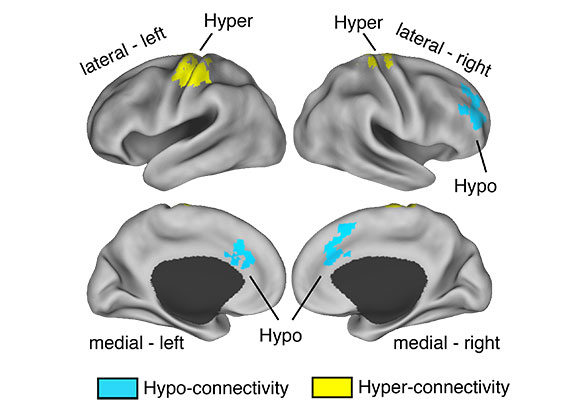
In an international multi-site study, researchers developed whole-brain functional connectivity maps of 243 people who experienced early warning symptoms and 154 healthy subjects, and then followed them for two years. They found a decrease in functional connectivity between the thalamus and prefrontal cortex regions in the at-risk group that was particularly pronounced in those who went on to develop full psychosis. However, the at-risk group also had excess connectivity between thalamus and sensory areas of the brain. This general pattern seen during these early stages of heightened risk resembled the changes seen in more chronic patients.
Cannon said more research needs to be done to definitively link disrupted functional connectivity between the thalamus and frontal cortex as a cause of schizophrenia. However, he noted that the study findings are consistent with the theory that those who develop schizophrenia experience an excessive reduction in synaptic connections between brain cells that normally occur during adolescence.
Reference: “Association of Thalamic Dysconnectivity and Conversion to Psychosis in Youth and Young Adults at Elevated Clinical Risk” by Alan Anticevic, Ph.D.; Kristen Haut, Ph.D.; John D. Murray, Ph.D.; Grega Repovs, Ph.D.; Genevieve J. Yang, BS; Caroline Diehl, BS; Sarah C. McEwen, Ph.D.; Carrie E. Bearden, Ph.D.; Jean Addington, Ph.D.; Bradley Goodyear, Ph.D.; Kristin S. Cadenhead, MD; Heline Mirzakhanian, Ph.D.; Barbara A. Cornblatt, Ph.D., MBA; Doreen Olvet, Ph.D.; Daniel H. Mathalon, MD, Ph.D.; Thomas H. McGlashan, MD; Diana O. Perkins, MD; Aysenil Belger, Ph.D.; Larry J. Seidman, Ph.D.; Ming T. Tsuang, MD, Ph.D., DSc; Theo G. M. van Erp, Ph.D.; Elaine F. Walker, Ph.D.; Stephan Hamann, Ph.D.; Scott W. Woods, MD; Maolin Qiu, Ph.D. and Tyrone D. Cannon, Ph.D., 12 August 2015, JAMA Psychiatry.
DOI:10.1001/jamapsychiatry.2015.0566








My name is Manuel Paulo; And I have been soufring with these disease since I Was Thirty years old, Now, Iam forty seven. I would like to know if in the next ten years I will have the total cure. To me the total cure include stop the medication once for all.
Today, people are 100% absolutely certain that schizophrenia is a mental illness. With this being the case, it is a fact that schizophrenia has been 100% surrounded or encompassed, otherwise it would be impossible to be 100% absolutely certain that schizophrenia is a mental illness in the first place.
With schizophrenia having been 100% encompassed, one clearly sees that which surrounds it, meaning one sees everything that schizophrenia is directly attached to. This of course includes seeing the very cause of schizophrenia itself. Therefore, this means that the cause of schizophrenia has been discovered.
However, if the cause has not been discovered as of yet, yet it is still being stated with 100% absolute certainty that schizophrenia is a mental illness, then this makes it crystal clear that society currently accepts/demands the idea that it is a fact that less than absolute always encompasses an absolute, meaning that it is currently accepted as fact that less than absolute is greater than absolute and thus it can and does encompass it.
This analysis is using pure logic. Via pure logic, for example, anyone who managed to pass grade 9 can discover entirely on their own, that which is described today as Albert Einstein’s special theory of relativity. You would have to be an absolute idiot not to be able to do so, or, as do over 99% of the population, you would have simply chosen to never accept nor use pure logic. https://www.youtube.com/watch?v=KKAwpEetJ-Q&list=PL3zkZRUI2IyBFAowlUivFbeBh-Mq7HdoQ