
Recent research led by Indiana University and the University of Chicago Medicine suggests that the drug α-difluoromethylornithine (DFMO) could revolutionize type 1 diabetes treatment. Building on a decade of studies, DFMO has demonstrated potential in reducing insulin dependency and is now being tested in a larger clinical trial to assess its impact on beta cell preservation and disease modification.
Recent research led by Indiana University School of Medicine in collaboration with the University of Chicago Medicine presents exciting future possibilities for the management of type 1 diabetes and the potential reduction of insulin dependency. The researchers’ findings, published in Cell Reports Medicine, suggest repurposing of the drug α-difluoromethylornithine (DFMO) may open doors to innovative therapies in the future.
Type 1 diabetes is a chronic condition wherein the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas, leading to high blood sugar levels that currently require lifelong insulin treatment to keep patients alive. Many people living with type 1 diabetes find current treatments, including daily insulin injections and frequent blood sugar monitoring, inconvenient and challenging to manage.
Decade-Long Research Journey
These latest translational results represent more than a decade of research. In 2010, the study’s co-corresponding author, Raghu Mirmira, MD, Ph.D., was operating a research lab at IU School of Medicine in 2010 when his team initially discovered that inhibiting the metabolic pathway affected by DFMO could safeguard beta cells from environmental factors, suggesting potential preservation in type 1 diabetes. The team subsequently validated these findings in mice.
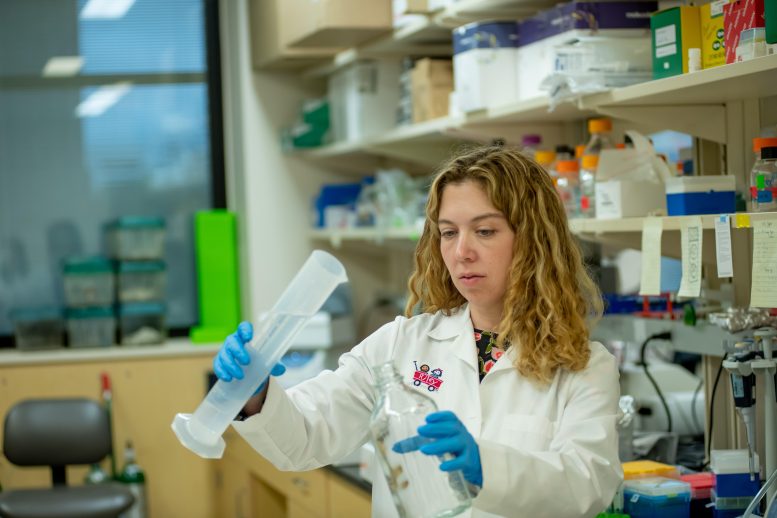
From 2015 to 2019, Linda DiMeglio, MD, MPH, Edwin Letzter Professor of Pediatrics at IU School of Medicine and a pediatric endocrinologist and division chief at Riley Children’s Health, directed a clinical trial that affirmed DFMO’s safety in people newly diagnosed with type 1 diabetes and suggested that it might also stabilize insulin levels by safeguarding beta cells. The trial was funded by the Juvenile Diabetes Research Foundation (JDRF) with a drug provided by Panbela Therapeutics.
“After several years of bench-to-bedside studies, beginning with Drs. Mirmira and [Sarah] Tersey’s mouse models, it’s exciting to finally share the promising results from our pilot trial in humans,” said DiMeglio, senior author of the study. “Now that we’ve established preliminary safety of DFMO for individuals with type 1 diabetes, we’re thrilled about advancing our collaborative research to explore more of its potential benefits in a larger clinical trial.”
DFMO’s Regulatory Advantages and New Formulations
Since 1990, DFMO has been FDA-approved as a high-dose injection to treat African Sleeping Sickness, and in 2020 it received a breakthrough therapy designation for neuroblastoma maintenance therapy after remission. This prior regulatory clearance could streamline its adoption as a type 1 diabetes treatment, potentially shortening the approval process from decades to just a few years.
“Using a new formulation of DFMO as a pill allows patients to take it by mouth instead of needing to undergo regular injections, and it has a very favorable side effect profile,” said Mirmira, who is now a professor of medicine and an endocrinologist at UChicago Medicine. “It’s exciting to say we have a drug that works differently from every other treatment we have for this disease.”
Ongoing and Future Clinical Studies
The researchers have already initiated their next steps in investigating DFMO’s potential. The study’s first author and co-corresponding author Emily K. Sims, MD, associate professor of pediatrics at IU School of Medicine and a pediatric endocrinologist at Riley Children’s Health, recently launched a larger, six-center clinical study to robustly define the impact of DFMO treatment to preserve beta cell function in type 1 diabetes. The new study is also funded by JDRF and supported by Panbela Therapeutics.
Sims, who is also a physician-scientist at the Herman B Wells Center for Pediatric Research and the Center for Diabetes and Metabolic Diseases at IU School of Medicine, is hopeful that DFMO, possibly as part of a combination therapy, will not only help persons recently diagnosed with type 1 diabetes but could also be tested in those at risk of developing the condition.
“As we dive into this new multicenter clinical trial to further investigate the efficacy of DFMO, we’re driven by the promising results we’ve seen so far to modify the underlying disease process in type 1 diabetes,” Sims said. “We invite more participants to join us in this pioneering research. With their help, the knowledge we gain today has the potential to shape a brighter future for those impacted by type 1 diabetes.”
Reference: “Inhibition of polyamine biosynthesis preserves β cell function in type 1 diabetes” by Emily K. Sims, Abhishek Kulkarni, Audrey Hull, Stephanie E. Woerner, Susanne Cabrera, Lucy D. Mastrandrea, Batoul Hammoud, Soumyadeep Sarkar, Ernesto S. Nakayasu, Teresa L. Mastracci, Susan M. Perkins, Fangqian Ouyang, Bobbie-Jo Webb-Robertson, Jacob R. Enriquez, Sarah A. Tersey, Carmella Evans-Molina, S. Alice Long, Lori Blanchfield, Eugene W. Gerner, Raghavendra G. Mirmira and Linda A. DiMeglio, 1 November 2023, Cell Reports Medicine.
DOI: 10.1016/j.xcrm.2023.101261
Individuals interested in learning more about the new clinical trial can visit the study’s website.







Be the first to comment on "Revolution in Diabetes Treatment: Repurposed Drug Shows Promise"