Rheumatoid arthritis is an autoimmune and inflammatory disease that causes joint inflammation and pain.
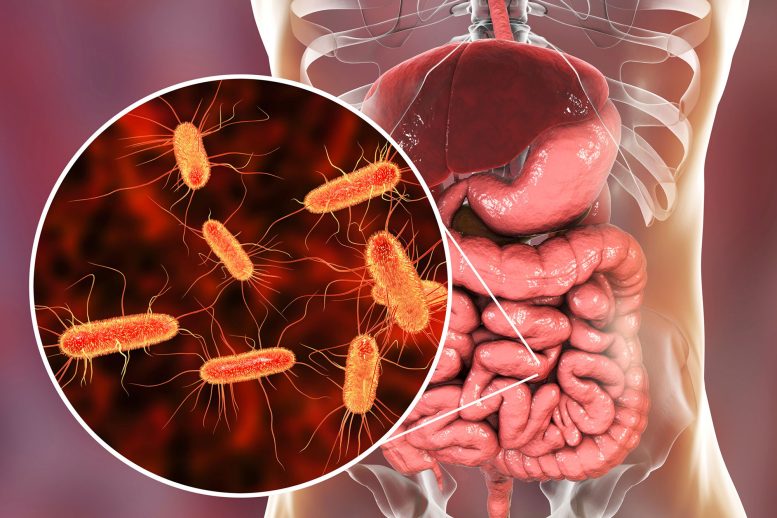
A bacterium has been identified by the CU Division of Rheumatology that may trigger rheumatoid arthritis in those who are already at risk.
Researchers at the University of Colorado School of Medicine have found that a unique bacteria found in the gut may be responsible for causing rheumatoid arthritis (RA) in patients who are already predisposed to the autoimmune disease.
A group of researchers from the Division of Rheumatology worked on the study under the leadership of Kristine Kuhn, MD, Ph.D., an associate professor of rheumatology. The study was recently published in the journal Science Translational Medicine. Meagan Chriswell, a medical student at CU, is the paper’s lead author.
“Work led by co-authors Drs. Kevin Deane, Kristen Demoruelle, and Mike Holers here at CU helped establish that we can identify people who are at risk for RA based on serologic markers, and that these markers can be present in the blood for many years before diagnosis,” Kuhn says. “When they looked at those antibodies, one is the normal class of antibody we normally see in circulation, but the other is an antibody that we usually associate with our mucosa, whether it be the oral mucosa, the gut mucosa, or the lung mucosa. We started to wonder, ‘Could there be something at a mucosal barrier site that could be driving RA?’”
Discovering a new bacterium
The CU researchers, with assistance from a team at Stanford University headed by Bill Robinson, MD, Ph.D., collected immune cells from people whose blood markers indicated they were at risk for the disease and mixed them with the at-risk people’s feces to discover the bacteria that were tagged by the antibodies.
The researchers employed animal models to host the newly found bacteria in order to explore their theory further. These tests revealed that the bacteria not only caused the animal models to develop the blood markers observed in people who are at risk for RA but that some of the models also developed full-blown RA.
“Our collaborators led by Drs. Eddie James and Jane Buckner of Benaroya Research Institute confirmed that the T cells in the blood of people with RA will respond to these bacteria, but people who are otherwise healthy do not respond to these bacteria,” Kuhn says. “Through studies in human and animal models, we were able to identify these bacteria as being associated with the risk for developing RA. They trigger an RA-like disease in the animal models, and in humans, we can show that this bacterium seems to be triggering immune responses specific to RA.”
A new target for RA
If the unique species of bacteria is indeed driving the immune response that leads to RA in individuals already at risk for the disease, Kuhn says, it might be possible to target the bacteria with medication to prevent that response from happening.
“The next thing we want to do is identify, in larger populations of individuals at risk for RA, if these bacteria correlate with other genetic, environmental, and mucosal immune responses, and then ultimately, the development of RA,” Kuhn says. “Then we could say, ‘This is a marker that’s useful in helping predict who will go on to develop RA,’ and apply prevention strategies. The other opportunity there is that if we can understand how it is triggering these immune responses, we might be able to block the bacteria’s ability to do that. “
Studying the trigger mechanism
The research took five years to conduct and analyze, Kuhn says, helped along by individuals who discovered they were at risk for RA and volunteered to support the research effort. Eventually, the researchers want to examine exactly how the bacteria triggers the immune response, as well as different methods of preventing the reaction from happening.
“There are a lot of different technologies that are just starting to come out that could selectively target a bacterium in the gut microbiome, for example, to prevent it from having immunogenic effects on the host,” she says. “For a long time, people have thought that antibiotics could be a useful therapy for RA, but rather than the sledgehammer effect of a traditional antibiotic that’s going to wipe out a large group of bacteria, we might be able to selectively target this bacterium or its effects.”
Reference: “Clonal IgA and IgG autoantibodies from individuals at risk for rheumatoid arthritis identify an arthritogenic strain of Subdoligranulum” by Meagan E. Chriswell, Adam R. Lefferts, Michael R. Clay, Alex Ren Hsu, Jennifer Seifert, Marie L. Feser, Cliff Rims, Michelle S. Bloom, Elizabeth A. Bemis, Sucai Liu, Megan D. Maerz, Daniel N. Frank, M. Kristen Demoruelle, Kevin D. Deane, Eddie A. James, Jane H. Buckner, William H. Robinson, V. Michael Holers and Kristine A. Kuhn, 26 October 2022, Science Translational Medicine.
DOI: 10.1126/scitranslmed.abn5166






I was discouraged to see they are still pushing a medication rather than just change diet. Steven Gundry is already fixing RA in patients via Dr diet change. The pill popping era is starting to be end.
Agree with you diet should be the first approach. My inflamed joints get set off by caffeine and artificial sweeteners. But probably a host of other things that I am unaware of.
I am suffering from an undefined auto immune disease and ther is always problem with my gut and full body arthritis.
Neurodivergent?
We have very similar issues. And I am neurodivergent.
Very informative.I much appreciated your study on the subject.
Over the last 4 years I have been seriously paying attention to my health. Doing everything that I can to fix my stomach, as an N.S.A.I.D. medication I was prescribed caused me to have a severe reaction in 2015 qnd almost caused my death.
I was diagnosed with R.A over 10 years ago. And also burcitus on my 5L lower back about 10 years ago.
With what I have learned from studying vigorously I have been taking baicalein, now I am wondering if this is the reason I no longer deal with both R.A. and burcitus.
Because that would make a whole lot of sense as I never even considered that those diagnosis could be created by a bacteria.
And that…. bacteria. Is what I have been fighting. .
Its been over 4 years now since I couldn’t sit up in bed because of burcirus.
Or I couldn’t walk because my knees hurt immensely.
I will have to keep informed about this. Because it would explane a lot.
How do we get that medicine I was diagnosed at 2 years old with thalassemia at 40 I have rheumatoid arthritis autoimmune disease osteoporosis and now they say I have IBS I’ve lost a lot of weight it would be nice if I could live the rest of my life with some kind of medicine that would take care of that thank you so much
It seems that medical medium was correct when he stated that it’s caused by bacteria or virus. Let’s keep looking at what’s in food as a source of triggers AND source of help
So happy to read studies are FINALLY looking into the RA/microbiome connection! Maybe within the next 20yrs scientists will show gut dysbiosis/ensuing inflammation at the core of a huge number of diseases afflicting an unhealthy American public. Western medicine more than happy to make millions on dangerous pharmaceuticals treating symptoms rather than research ways to eradicate disease. 😭
Been suffering reactive arthritis since my 20’s. Discovered in my mid 30’s that antibiotics made it better. Wish I had another choice but nothing offered thus far.
A disease always starts in the gutt. I am glad some solid research is getting done.
Years ago I read an article about a doctor who correlated bacteria with arthritis. I’m a CNA. Undereducated but I overly research. My grandmother had severe arthritis. That article stayed with me and in pursuit of early onset arthritis due to debilitating car wrecks, I am about to put myself on a maintenance dose. Yes, I know they are now saying there is an increase of colon cancer with antibiotics but screening and a low dose should help that. I have a 91 year old healthy as a hog wart gentleman on a maintenance dose.
This is some great information to read! I was diagnosed with RA as a teen and have had it for so many years. I want to know what I can take to stop from this RA from damaging my Joints More? I never read what you suggest RA people to take to ease or even put the RA into remission? Is there any hope for us with autoimmune diseases? I’m So tired of this RA! I’ve been doing infusions to suppress my immune system for over 15 years, & NSAID’s & not e anti-inflammatory prescriptions, and I’m tired of having to take all these prescriptions. I don’t try to eat nightshade vegetables, sweet’s, wheat, dairy, etc. Please Help me!
Bacteria that caused my arthritis and FL romialgya were in three INFECTED ROOT CANA. I AM NOW FREE OF PAIN AND INFLAMATION AFTER THE ROOT CANALS EXTRACTION BY A BILIGICALVDENTIST.
To anyone dealing with these type of underlying conditions, I would highly suggest having a 24 hour oxalate urine test performed. It is obviously non-invasive but can indicate primary or secondary hyperoxaluria. Essentially, your body either produces extra or lacks enough of the appropriate gut bacteria, to break down oxalic acids, which aggregate and aggravate all of the above mentioned symptoms. If you are eating foods that are particularly high in oxalates, it can make your symptoms worse. The oxalates deposit in your body, and cause autoimmune issues. I suspected that I had this.I out myself on a lower oxalate diet, added supplements that allowed oxalates in my plant foods, to bind to them so that I could essentially excrete them out, opposed to them migrating into different parts of my body via the wide junctions left open from inflammation in my gut mucosa. I reversed most of my anemia, passed a kidney stone and reversed my hyperlipedemia. My doctor hadn’t heard of this so he sent me to a Urologist and sent me for a 24 hr oxalate test. I went off my diet and protocol for 3 days, to achieve a baseline and took the urine test. I was diagnosed with secondary hyperoxaluria. The Urologist approved my protocol and confirmed through a CT, that I had passed a 3mm stone. I am being evaluated for IBD, PAH, pulmonary fibrosis, and a myriad of other conditions. I have been able to halt the progression and reverse some of my issues with the changes I have made in the last three months. Gut microbiota is everything. I started taking different probiotics with prebiotic foods and it has made a difference. No one ever warned me that I could have hyperoxaluria. I am also neurodivergent. There are a ton of studies showing a high correlation of hyperoxaluria in patients with ADHD and autism. The calcium oxalate crystals are bifringent and embed themselves in joint synovial fluids, interstitial fluids in lungs, your heart, your kidneys ( calcium oxalate stones) and cause neuro hypersensitivity. Imagine microscopic shards of glass…that is how they act. They mitigate and amplify inflammation and oxidative stress.
Have the urine test. It is worth knowing if you have the condition because you can treat it.
I tried absolutely every “healthy” thing I could. Detoxing and juicing spinach. Ironically, spinach has the highest concentration of oxalates out of any food we could eat.
This is what I can contribute to this conversation.
Agreed. Not beholden to one type of tmt. However, I can document the moon is made out of green cheese. Point? Antecdotal accounts need double blind studies.
@Brenda- my family has thalassemia as well. It’s like sickle cell anemia except this version is found in Mediterranean decent as I understand it. One of my family members takes ferritin. She needs the ferritin form of iron. Prior to that she was told she was so anemic that if she cut herself she would die. She’s taken ferritin for years and is fine.
Has this research found any connection or correlation to gluten and celiac disease? So many of my issues cleared up when I went gluten free after being diagnosed via genetic test and endoscopy. By then I had severe flattening of microvilli in my small intestine (could not even be detected by micro camera) and 4 months later perforation of my small intestine. Obviously things had been deteriorating for some time before light bulb went on with my preferred provider.
Big pharma funds a lot of these studies looking for profit margin when people have illnesses that can be exploited for long term management! Chris Rock put it best, “money’s in the treatment not the cure!”
Interesting! I accidentally found out that milk was causing my joint pain and inflammation. Take care of your belly and your belly will take care of you 🙂 Also, read SciTech daily lol 🤣
Diagnosed at 64 Started on the Pattison diet, non-inflammatory Foods. Worth looking into. I feel it’s helping also taking methotrexate and prednisone in the meantime.
Treatment of inflammatory bowel disease: Potential effect of NMN on intestinal barrier and gut microbiota.
https://www.sciencedirect.com/science/article/pii/S2665927122001289
Please correct the title: “an unique gut bacterium”.
Hi I have rheumatoid arthritis since 2000. It started after I were armed robbed. I had operations on my toes. My one hand has deformity fingers. I do gym and that helps me to go on. I pray that they get a cure for future people to get this illness. 🙏
I have been suffering now with arthritis all throughout my spine my l5 did not finish developing so I have arthritis in my lower lumbar and also degenerative disc disease but arthritis in my hands my feet my knees my ankles all over I have not changed my diet I was taking celebrex but they took me off of that because my blood is starting to thicken. I have bursitis also in my shoulders and in my neck and I have had surgery on both I would love to know more about this medication I am only 54 years old and have been suffering with this arthritis since I was around 48 it is only gotten worse. I cannot even work anymore because of the arthritis and bursitis and they have diagnosed me with fibromyalgia also .
I have arthritis in my back and joints,I visited thepeopleschemist.com and found immune fx,joint fx.these products have given me my movement and life back.i suffered from gut issues before taking immune fx,now gut issues are gone.the natural ingredients in immune fx are nature’s antibiotics. Please consider taking these products before any medications, these products saved my life.good luck
I wish they’d cited the genus and species of which bacterium they are referring to in the article. It leads me to suspect some big pharma patent issues may be invoved. Why else be so secretive.