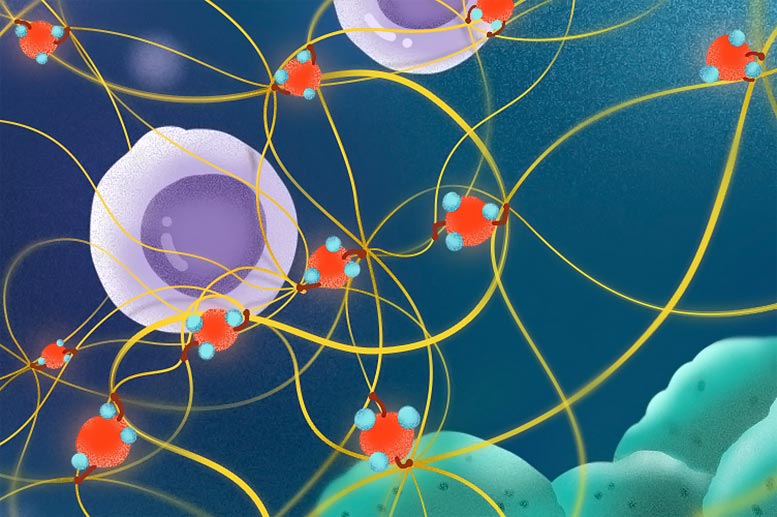
Inhaled fine particulate matter (shown here in red) pulls strings of collagen to disturb the immune defense in mice with lung cancer cells. This activity delays the movement of cytotoxic T-cells (purple) as they migrate towards the cancer cells (green) to destroy them. Credit: Wang et al. (CC BY 4.0)
Research findings highlight a potential new target for preventing lung disease caused by air pollution.
According to a paper published in the journal eLife on April 19, 2022, scientists have uncovered a mechanism that explains how small air pollution particles may induce lung cancer.
The discovery could pave the way for novel techniques to prevent or treat the early lung alterations that lead to the disease.
Tiny, inhalable fine particulate matter (FPM) found in air pollutants has been recognized as a Group 1 carcinogen and a substantial threat to global health. However, the cancer-causing mechanism of FPM remains unclear.
“Despite its potential to cause mutations, recent research suggests that FPM does not directly promote – and may even inhibit – the growth of lung cancer cells,” explains first author Zhenzhen Wang, an associate researcher at Nanjing University (NJU), Nanjing, China, who carried out the study between labs at NJU and the University of Macau where she was sponsored by a University of Macau Fellowship. “This suggests that FPM might lead to cancer through indirect means that support tumor growth. For example, some studies suggest FPM can prevent immune cells from moving to where they are needed.”
To explore this possibility, Wang and the team collected FPM from seven locations in China and studied its effects on the main immune cells that defend against tumor growth – called cytotoxic T-cells (CTLs). In mice administered with lung cancer cells that were not exposed to FPM, CTLs were recruited to the lung to destroy the tumor cells. By contrast, in the mice whose lungs were exposed to FPM, the infiltration of CTLs was delayed – potentially allowing the tumor cells to establish in lung tissue.
To investigate why the CTLs did not enter the lung as quickly in the FPM-exposed lungs, the research team studied both the CTLs themselves and the lung tissue structure. They found that CTLs exposed to FPM still retained their migratory ability, but that FPM exposure dramatically compressed the lung tissue structure and the spaces that immune cells move between. There were also much higher levels of collagen – a protein that provides biomechanical support for cells and tissues. When the scientists studied the movement of CTLs in the mice, in lung tissue exposed to FPM, CTLs struggled to move. However, those in the untreated tissue were able to move freely.
Further analysis of the tissue showed that the structural changes were caused by increases in a collagen subtype called collagen IV, but the researchers still did not know how FPM triggered this. They found the answer when they looked more closely at the structural changes to collagen IV and the enzyme responsible for making them – called peroxidasin. This enzyme drives a specific type of cross-linking that exposure to FPM was found to cause and aggravate in the lung tissue.
“The most surprising find was the mechanism by which this process occurred,” Wang says. “The peroxidasin enzyme stuck to the FPM in the lung, which increased its activity. Taken together, this means that wherever FPM lands in the lung, increased peroxidasin activity leads to structural changes in the lung tissue that can keep immune cells out and away from growing tumor cells.”
“Our study reveals a completely new mechanism by which inhaled fine particles promote lung tumor development,” concludes senior author Lei Dong, Professor at the School of Life Sciences, Nanjing University. “We provide direct evidence that proteins that stick to fine particulate matter can cause a significant and adverse effect, giving rise to pathogenic activity. Our discovery that peroxidasin is the mediator of this effect in lung tissue identifies it as a specific and unexpected target for preventing lung disease caused by air pollution.”
Reference: “Air pollution particles hijack peroxidasin to disrupt immunosurveillance and promote lung cancer” by Zhenzhen Wang, Ziyu Zhai, Chunyu Chen, Xuejiao Tian, Zhen Xing, Panfei Xing, Yushun Yang, Junfeng Zhang, Chunming Wang and Lei Dong, 19 April 2022, eLife.
DOI: 10.7554/eLife.75345




Be the first to comment on "Scientists Discover How Air Pollution Alters Lung Tissue, Increasing Cancer Susceptibility"