
Northwestern Medicine scientists have made a groundbreaking discovery that redefines our understanding of how antipsychotic drugs work, revealing that their interaction with D1 dopamine receptor-expressing neurons, not D2, better predicts their efficacy in treating schizophrenia.
New research finding about how drugs modulate the brain in schizophrenia could lead to better treatments.
Antipsychotic drugs used to treat the millions of people in the U.S. diagnosed with schizophrenia often have numerous undesirable side effects. Additionally, these drugs are ineffective for many individuals, leading to an urgent requirement for the development of more efficacious drugs.
New Approach for Drug Development
Northwestern Medicine scientists have uncovered a promising pathway for creating more effective treatments for the crippling symptoms of schizophrenia. Traditionally, researchers have screened antipsychotic drug candidates by observing their effects on mouse behavior. However, the innovative approach adopted by a Northwestern lab has proven to be superior in predicting the drugs’ effectiveness in patients.
The study discovered that antipsychotic drugs – which inhibit the overactive dopamine causing the symptoms of schizophrenia – interact with a completely different neuron than scientists originally believed.
“This is a landmark finding that completely revises our understanding of the neural basis for psychosis and charts a new path for developing new treatments for it,” said lead investigator Jones Parker, assistant professor of neuroscience at Northwestern University Feinberg School of Medicine.” It opens new options to develop drugs that have fewer adverse side effects than the current ones.”
The study was published on July 13 in the journal Nature Neuroscience.
Understanding Dopamine’s Role
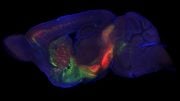
Schizophrenia patients have elevated dopamine levels in a brain region called the striatum, which hosts two primary types of specialized brain cells or neurons. These cells are distinguished by the type of dopamine receptor they possess: D1 and D2.
Receptors on neurons are like locks waiting for the key that turns them on. Picture two populations of neurons, one that expresses locks called D1 receptors and the other called D2 receptors. Dopamine is a key for both receptors, but antipsychotics only block the D2 receptor locks. Therefore, experts have assumed these drugs preferentially act on neurons that express the D2 receptor locks. But, in fact, it was the other brain cells – the neighboring ones in the striatum with D1 receptors – that responded to antipsychotic drugs in a manner that predicted clinical effect.
Shifting the Paradigm
“The dogma has been that antipsychotic drugs preferentially affect striatal neurons that express D2 dopamine receptors,” Parker said. “However, when our team tested this idea, we found that how a drug affects the activity of D2 receptor-expressing striatal neurons has little bearing on whether it is antipsychotic in humans. Instead, a drug’s effect on the other striatal neuron type, the one that expresses D1 dopamine receptors, is more predictive of whether they actually work.”
Limitations of Current Treatments
Schizophrenia is a debilitating brain disorder affecting roughly 1 in 100 people or more than 2.5 million people in the U.S. While existing antipsychotics are effective for the hallmark symptoms of schizophrenia such as hallucinations and delusions, they are ineffective for the other symptoms of schizophrenia such as deficits in cognitive and social function.
Furthermore, current antipsychotics are completely ineffective in more than 30% of patients with treatment-resistant schizophrenia (more than 750,000 people in the U.S.). The use of these drugs also is limited by their adverse effects, including tardive dyskinesia (uncontrollable body movements) and parkinsonism (rigidity, tremors, and slowness of movement).
Novel Insights and Future Directions
The new study for the first time determined how antipsychotic drugs modulate the region of the brain thought to cause psychosis in living animals.
“Our study exposed our lack of understanding for how these drugs work and uncovered new therapeutic strategies for developing more effective antipsychotics,” Parker said.
Reference: “Antipsychotic drug efficacy correlates with the modulation of D1 rather than D2 receptor-expressing striatal projection neurons” by Seongsik Yun, Ben Yang, Justin D. Anair, Madison M. Martin, Stefan W. Fleps, Arin Pamukcu, Nai-Hsing Yeh, Anis Contractor, Ann Kennedy and Jones G. Parker, 13 July 2023, Nature Neuroscience.
DOI: 10.1038/s41593-023-01390-9
Other Northwestern authors include first author Seongsik Yun, Ben Yang, Justin Anair, Madison Martin, Stefan Fleps, Arin Pamukcu, Nai-Hsing Yeh, Anis Contractor, and Ann Kennedy.
The research was supported by the National Institute of Neurological Disorders and Stroke grant R01NS122840 and the National Institute of Mental Health grant K01MH11313201, both of the National Institutes of Health and the Whitehall Foundation.






Be the first to comment on "Shattering Old Beliefs: Antipsychotic Drugs Work Differently Than Scientists Thought"