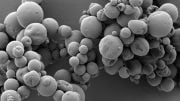
Scientists developed a new technique to identify and quantify viral RNA in living cells, detecting even minor sequence changes that could impact virus behavior or contribute to certain individuals becoming “superspreaders.”. Credit: American Chemical Society
Studying viral outbreaks in single cells could reveal new ways to defeat them.
Many viruses, including HIV and influenza A, mutate so quickly that identifying effective vaccines or treatments is like trying to hit a moving target. A better understanding of viral propagation and evolution in single cells could help. Today, scientists report a new technique that can not only identify and quantify viral RNA in living cells, but also detect minor changes in RNA sequences that might give viruses an edge or make some people “superspreaders.”
The researchers presented their results at the American Chemical Society (ACS) Fall 2020 Virtual Meeting & Expo. It featured more than 6,000 presentations on a wide range of science topics.
A brand-new video about the research is available here:
“For studying a new virus like SARS-CoV-2, it’s important to understand not only how populations respond to the virus, but how individuals – either people or cells – interact with it,” says Laura Fabris, Ph.D., the project’s principal investigator. “So we’ve focused our efforts on studying viral replication in single cells, which in the past has been technically challenging.”
Analyzing individual cells instead of large populations could go a long way toward better understanding many facets of viral outbreaks, such as superspreaders. That’s a phenomenon in which some cells or people carry unusually high amounts of virus and therefore can infect many others. If researchers could identify single cells with high viral loads in superspreaders and then study the viral sequences in those cells, they could perhaps learn how viruses evolve to become more infectious or to outwit therapies and vaccines. In addition, features of the host cell itself could aid various viral processes and thus become targets for therapies. On the other end of the spectrum, some cells produce mutated viruses that are no longer infectious. Understanding how this happens could also lead to new antiviral therapies and vaccines.
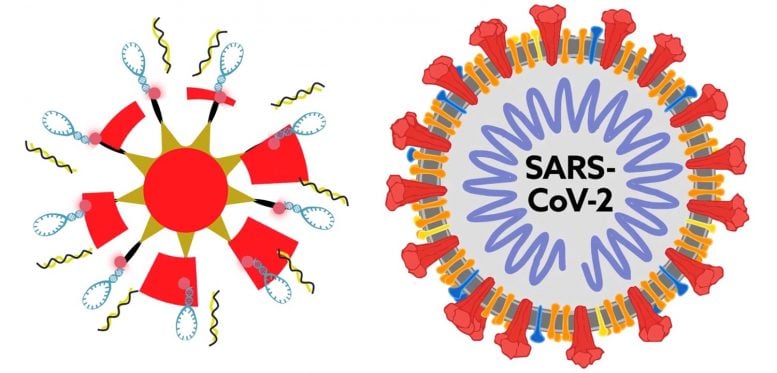
But first, Fabris and colleagues at Rutgers University needed to develop an assay that was sensitive enough to detect viral RNA, and its mutations, in single living cells. The team based their technique on surface enhanced Raman spectroscopy (SERS), a sensitive method that detects interactions between molecules through changes in how they scatter light. The researchers decided to use the method to study influenza A. To detect the virus’s RNA, they added to gold nanoparticles a “beacon DNA” specific to influenza A. In the presence of influenza A RNA, the beacon produced a strong SERS signal, whereas in the absence of this RNA, it did not. The beacon produced weaker SERS signals with increasing numbers of viral mutations, allowing the researchers to detect as few as two nucleotide changes. Importantly, the nanoparticles could enter human cells in a dish, and they produced a SERS signal only in those cells expressing influenza A RNA.
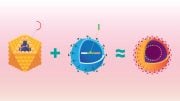
Now, Fabris and colleagues are making a version of the assay that produces a fluorescent signal, instead of a SERS signal, when viral RNA is detected. “SERS is not a clinically approved technology. It’s just now breaking into the clinic,” Fabris notes. “So we wanted to provide clinicians and virologists with an approach they would be more familiar with and have the technology to use right now.” In collaboration with virologists and mathematicians at other universities, the team is developing microfluidic devices, or “lab-on-a-chip” technologies, to read many fluorescent samples simultaneously.
Because SERS is more sensitive, cheaper, faster, and easier to perform than other assays based on fluorescence or the reverse transcriptase-polymerase chain reaction (known as RT-PCR), it could prove ideal for detecting and studying viruses in the future. Fabris is now collaborating with a company that makes a low-cost, portable Raman spectrometer, which would enable the SERS assay to be easily conducted in the field.
Fabris and her team are also working on identifying regions of the SARS-CoV-2 genome to target with SERS probes. “We’re in the process of obtaining funding to work on possible SARS-CoV-2 diagnostics with the SERS method we developed,” Fabris says.
The researchers acknowledge support and funding from the Defense Advanced Research Projects Agency.




Be the first to comment on "Studying the Genetic Evolution of Viruses Like SARS-CoV-2 in Single Cells Could Reveal New Ways to Defeat Them"