
Dr. Hooley and Dr. Mazure with the tools used for supplementary ultrasound screening. Credit: Michael Marsland
New research shows that a supplementary screening with ultrasound can detect cancers missed by mammography, and reveals that women with dense breast tissue can benefit from this extra screening.
The purpose of screening examinations for breast cancer is to detect tumors before they cause symptoms such as a lump, swelling, or redness. Discovering tumors in their early stages is key to reducing breast cancer mortality because they are still small and can be treated before they spread beyond the breast.
Once breast cancer has metastasized, treatments can delay the progression of the disease and extend survival but it is not always a curable condition.
This, along with the fact that breast cancer risk can increase with age, is why the American Cancer Society recommends an annual mammogram, an X-ray image of the breast, for women 40 and older. Thus far, mammography is the only screening method proven in clinical studies with women volunteers to reduce the number of deaths from breast cancer through early detection.
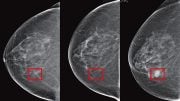
However, mammography has its limitations and is an imprecise screening method that can miss breast cancers in some women, especially those with dense breast tissue. In addition, having dense breast tissue is linked to a higher risk of breast cancer compared to the risk for women without dense tissue.
Breasts consist of a mixture of fatty, glandular, and fibrous connective tissue, and the composition varies among women. On mammography in women without dense breast tissue, tumors usually appear white against a gray background of fatty tissue. However, in women with dense breasts, there is more glandular and connective tissue which appears as a white background, making it more difficult to spot a tumor. As Dr. Regina Hooley puts it, “It’s like looking for a polar bear in a snowstorm.”
Women’s Health Research at Yale awarded Hooley, Associate Professor of Diagnostic Radiology and a clinician at the Smilow Breast Center, a 2012 Pilot Project Program grant to conduct one of the first studies in the nation on the performance and value of supplementing mammography with ultrasound screening, a method that uses sound waves to produce an image of the breast.
She completed her study earlier this year and found that supplementary screening with ultrasound can detect cancers missed by mammography. Her results indicate that women with dense breast tissue can benefit from this extra screening and often will choose the screening if made aware of their breast density.
IS THERE VALUE TO MAMMOGRAPHY PLUS ULTRASOUND?
“When used to supplement mammography, breast ultrasound’s cancer detection rate is approximately 3 cancers per 1,000 women screened, as compared to approximately 5 new cases per 1,000 women screened with mammography,” Hooley said. “I definitely think breast ultrasound screening is beneficial, and women who are informed about breast density appreciate that they have the choice to supplement their mammogram.”
The main element of Hooley’s study was a review of the records of approximately 4,000 women who visited the Smilow Breast Center for mammography and supplementary ultrasound screening in the first three years, 2009 to 2012, after a Connecticut state law on breast density notification took effect.
The law requires radiologists to inform women who undergo mammography if they have dense breast tissue and that they may benefit from supplementary screening tests. Before the mandate, the clinic did not offer ultrasound screening. However, upon the mandate’s implementation, the clinic began offering ultrasound screening by trained technicians using hand-held devices.
First, the records of 935 women who had supplemental screening showed that ultrasound testing detected 3 cancers per 1,000 screened.
Next, Hooley reviewed the records of 1,046 women who underwent supplementary ultrasound screening after the clinic began using a new, more sophisticated mammography (tomosynthesis, which provides three-dimensional images) along with regular mammography. This allowed her to compare the detection rate using supplemental ultrasound screening for traditional mammography versus tomosynthesis.
Not surprisingly, because the 3-D mammograms revealed cancers at a higher rate than regular mammograms, the detection rate for supplementary screening with ultrasound decreased to just under 2 cancers per thousand.
PATIENTS’ VIEWS
Hooley’s pilot study also was designed to determine patients’ opinions about ultrasound screening and breast density.
A questionnaire was distributed to 950 women with dense breast tissue who had come to the center for breast screening tests between January and October 2013. Completed surveys were collected from 803 of these women. Their average age was 53. Their answers showed that:
- 92 percent were aware of their breast density and 89 percent had been informed of their dense breast tissue based on mammography.
- 41 percent reported increased anxiety due to knowing about their breast density.
- 77 percent reported having at least one prior breast ultrasound screening exam.
- 73 percent chose to have breast ultrasound screening based on their primary health care provider’s advice.
- 90 percent reported they chose to have ultrasound screening despite the increased chance of needing additional testing and, perhaps a biopsy, after the screening.
Hooley noted that the survey results cannot represent the views of all women in that there are no data on those who do not routinely participate in mammography or supplemental ultrasound screening.
THE ISSUE
Connecticut was the first state to enact a breast-density notification law. In addition to mandating that women undergoing mammography be informed if they have dense breasts, the law requires radiology facilities to inform their patients that breast ultrasound screening and MRI examinations are options as supplemental tests. An MRI (magnetic resonance imaging) test requires an intravenous contrast agent and uses a magnetic field and radio waves to create images, Hooley explained.
Since 2011, 18 other states have adopted similar breast-density notification laws. Federal breast-density notification legislation was introduced earlier this year in the U.S. Senate by California Sen. Diane Feinstein and New Hampshire Sen. Kelly Ayotte, and in the U.S. House of Representatives by Connecticut Rep. Rosa L. DeLauro and New York Rep. Steve Israel.
With Connecticut having a head start on the rest of the nation, Hooley’s WHRY-funded study has been the leading edge of a growing medical debate that has become a national issue.
Critics of the breast-density notification laws point to a high rate of false positives with ultrasound screening, leading to unnecessary biopsies. They say supplemental screening with ultrasound has yet to be proven as beneficial and cost-effective.
The laws’ supporters say that women should be informed if they have dense breast tissue and made aware that supplementary screening options are available. They say that, as radiologists gain experience with supplemental screening with ultrasound, false positives can be reduced and that finding cancers at a smaller size and earlier stage can reduce breast cancer deaths.
Based on her WHRY-funded study results and the increasing number of states that have enacted breast density notification laws, Hooley said she views ultrasound screening after mammography as a supplementary breast cancer screening option that is here to stay, even with the use of the more sophisticated three-dimensional mammography. She cautioned, however, that her study focused on a relatively small population over a three-year period.
“I think we have a lot to investigate further, in terms of larger populations and longer periods of time, when we are talking about a national policy,” Hooley said.
The rate of false positives is being reduced as radiologists in the Smilow clinic gain more experience interpreting ultrasound images. With the increasing experience using the hand-held devices, she said, clinicians are learning to recognize benign masses that do not need additional testing.
“I think the potential for ultrasound (screening) is still untapped,” she said. “It’s really a work in progress, and this study funded by Women’s Health Research at Yale has provided some of the first data to demonstrate its value.”







Be the first to comment on "Ultrasound Can Detect Cancers Missed by Mammography"