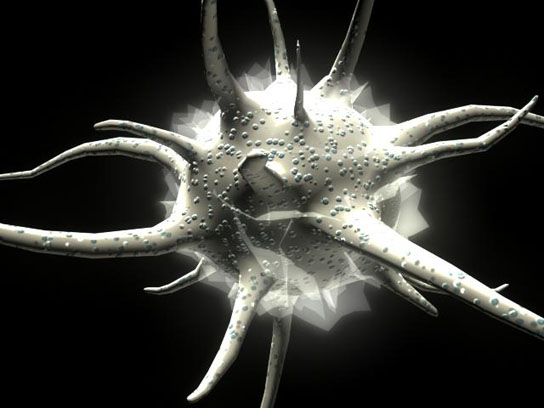
Dendritic Cell. Credit: David Hunt
A groundbreaking dendritic cell vaccine study is underway at the Center for Immunotherapy at Roswell Park Cancer Institute. Researchers at RCPI began a phase 1 clinical research study of the NY-ESO-1dendritic cell vaccine. This is the first facility in the world using an FDA-approved process in a government-regulated study. The hope is that this vaccine will eradicate cancer cells and prevent disease relapse in patients.
The Center for Immunotherapy at Roswell Park Cancer Institute (RPCI) has launched a phase I clinical research study of a dendritic cell vaccine designed to both eradicate cancer cells and prevent disease relapse. Developed at RPCI, the NY-ESO-1 dendritic cell vaccine will be manufactured in the Institute’s new Therapeutic Cell Production Facility using a unique FDA-approved process — making RPCI the first research facility in the U.S. to use a custom-made barrier isolator for vaccine cell production, and the first in the world to use this system in an approved, government-regulated study.
Dendritic cells are the gatekeepers of the human immune system, defending against invaders like bacteria, viruses and cancer. The vaccine to be produced at RPCI will be the first to incorporate a particular form of NY-ESO-1, antiDEC205-NY-ESO-1. “Armed with this specialized protein, the treated cells are then given back to the patient as a vaccine designed to recruit an army of killer immune cells that seek out and destroy cancer,” explains Kunle Odunsi, MD, PhD, Director of RPCI’s Center for Immunotherapy (CFI) and the study’s Principal Investigator.
The new study is also unique in that it’s the first to test a dendritic vaccine given in combination with rapamycin, a compound used to prevent rejection of solid-organ transplant. The study just launched will capitalize on a striking recent scientific discovery by Protul Shrikant, PhD, of the Department of Immunology at RPCI, who found that in low doses, rapamycin confers a previously unknown benefit — it prevents the immune system from using up its cancer-killing T-cells in one quick burst. “We have shown for the first time that rapamycin has the capacity to produce immune cells that have memory attributes,” explains Dr. Odunsi, who is also Chair of RPCI’s Department of Gynecologic Oncology. “The immune cells are trained to live longer and to always remember that cancer cells are bad and should be attacked and killed.”
The ability to stretch out the attack for a long-term, durable response suggests that the vaccine may be effective in preventing disease recurrence. The new NY-ESO-1 dendritic cell vaccine is expected to show great promise in patients with bladder, brain, breast, esophageal, gastrointestinal, hepatocellular, kidney, lung, melanoma, ovarian, prostate, sarcoma, and uterine tumors.
The NY-ESO-1 vaccine, tailor-made for each patient, will be produced in RPCI’s Therapeutic Cell Production Facility (TCPF) under the direction of Yeong “Christopher” Choi, PhD, who notes: “We believe that our facility’s custom-made barrier isolator, the unit in which the vaccines are manufactured, is the first of its kind.” The barrier isolator — an Xvivo System processing chamber designed to RPCI’s specifications by BioSpherix, Ltd., Lacona, NY — maintains strict control of the unit’s temperature and atmospheric gases, critical for optimal production of dendritic cell vaccines.
“Those conditions, and the sterile vaccine-manufacturing environment, are rigidly maintained throughout the entire process,” says Dr. Choi. “The Xvivo — which at about 70 square feet is basically a clean room in a box — acts as a physical barrier that protects the cell-therapy product from outside contaminants, resulting in a safer, more predictable manufacturing process.”
The potential of therapeutic vaccines is attracting increasing interest in the field of oncology. Last year, the FDA approved the first therapeutic cancer vaccine, Provenge® (sipuleucel-T), for men with advanced prostate cancer. RPCI’s Center for Immunotherapy is awaiting FDA approval to launch additional cancer vaccine trials, including a vaccine for malignant glioma (a type of brain tumor) and another vaccine for patients with ovarian, fallopian tube, and primary peritoneal cancer.
“This trial will be only the beginning of a very robust program of activity in the area of using the human immune system to fight cancer,” adds Dr. Odunsi. “Our production process holds tremendous potential for applications related to stem-cell therapy and regenerative medicine, and I believe we’re uniquely positioned at RPCI to have the tools, infrastructure, and multidisciplinary collaboration to capitalize on these ideas and opportunities both effectively and efficiently.”
The clinical research study will enroll 18-20 eligible patients whose tumors express a specific antigen, known as NY-ESO-1. Apart from the adult male testis, NY-ESO-1 is not expressed in normal tissues of the body, but is expressed in cancers. This may help decrease the risk of side effects from the vaccine, because it should target only the tissues that express NY-ESO-1.
Dr. Odunsi, who developed the NY-ESO-1 vaccine, led previous trials evaluating its effectiveness in treating ovarian cancer. Christine Sable of Lancaster, Pennsylvania, enrolled on one of those studies in February of 2004, after undergoing surgery and chemotherapy for advanced-stage ovarian cancer. Although she faced a 75-80% chance that the cancer would return, her immune system responded strongly to the vaccine, and she has remained cancer-free in the seven years since then, with no side effects.




Be the first to comment on "RPCI Facility Begins Research Study of a Dendritic Cell Vaccine"