A research team found that exosomes from γδ-T cells can enhance radiotherapy’s effectiveness against nasopharyngeal carcinoma (NPC) by overcoming the cancer stem cells’ resistance.
HKUMed develops a novel therapeutic approach against nasopharyngeal carcinoma by using exosomes derived from γδ-T cells synergized with radiotherapy
A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that exosomes derived from γδ-T cells (γδ-T-Exos) synergised with radiotherapy can control nasopharyngeal carcinoma (NPC) by overcoming the radioresistance of NPC cancer stem cells (CSCs) and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. This study provides a proof of concept for a novel and potent strategy by combining γδ-T-Exos with radiotherapy in the control of NPC. The groundbreaking research was published in the prestigious academic journal Journal of Immunotherapy of Cancer.
Background
Nasopharyngeal carcinoma (NPC) is one of the most aggressive Epstein-Barr virus (EBV)-related tumors and is very prevalent in East Asia, including Hong Kong. Although radiotherapy is the first-line treatment for NPC, its therapeutic efficiency is limited in some patients due to radioresistance. Adoptive T cell immunotherapy has also shown promise in the treatment of NPC; however, its anti-tumor effectiveness may be hampered by an immunosuppressive tumor microenvironment. Exosomes are microscopic extracellular vesicles that originate in the endosome and promote intercellular communication. Cell-free exosomes provide higher safety, simpler storage, and cheaper costs than cell-based therapy. Researchers previously established that γδ-T-Exos might successfully limit the progression of EBV-associated tumors in a previous study. However, it remains unknown whether γδ-T-Exos have a synergistic effect with radiotherapy and preserve their anti-tumor activities against NPC in an immunosuppressive tumor microenvironment.
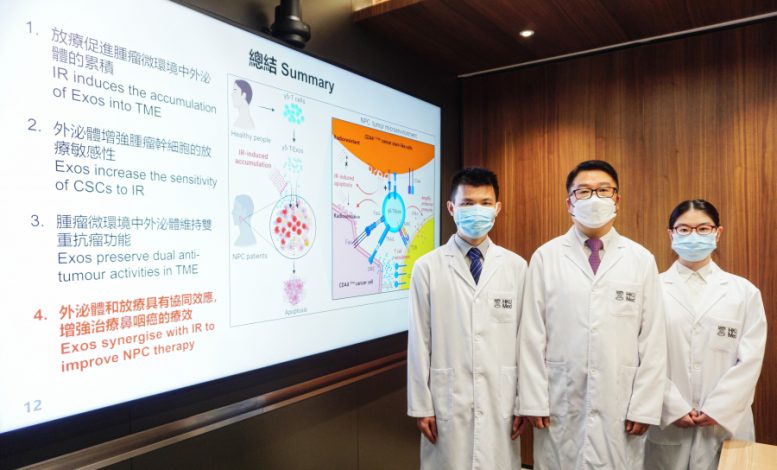
HKUMed develops a novel therapeutic approach against nasopharyngeal carcinoma by using exosomes derived from γδ-T cells synergize with radiotherapy. The research was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed (middle), and Dr. Wang Xiwei, post-doctoral fellow of Professor Tu’s team (left), is the first author. PhD student Zhang Yanmei (right) is a member of the research team. Credit: The University of Hong Kong
Research findings
Herein, the research team found that γδ-T-Exos not only effectively interacted with NPC cells and induced tumor cell death in vitro, which was mainly mediated by Fas/Fas ligand (FasL) and death receptor 5 (DR5)/tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) pathways, but also controlled NPC tumor growth and prolonged tumor-bearing mice survival in vivo. Furthermore, γδ-T-Exos selectively targeted the radioresistant CD44+/high CSCs and induced profound cell apoptosis. The combination of γδ-T-Exos with radiotherapy overcame the radioresistance of CD44+/high NPC cells and significantly improved its therapeutic efficacy against NPC in vitro and in vivo. In addition, γδ-T-Exos promoted T-cell migration into NPC tumors by upregulating CCR5 on T cells that were chemoattracted by CCR5 ligands in the NPC tumor microenvironment. Although NPC tumor cells secreted abundant tumor growth factor beta (TGF-β) to suppress T- cell responses, γδ-T-Exos preserved their direct anti-tumor activities and overcame the immunosuppressive NPC microenvironment to amplify T-cell anti-tumor immunity.
‘Our study first provides a strong pre-clinical proof of concept using a novel therapeutic strategy by combining γδ-T-Exos with radiotherapy to treat NPC. γδ-T-Exos can effectively interact with and kill both EBV positive and negative NPC cells. More importantly, γδ-T-Exos can eradicate radioresistant NPC CSCs and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. Therefore, combination of radiotherapy with γδ-T- Exos has great potential in the treatment of NPC, which will be highly beneficial to the clinical application of this approach,’ said Professor Tu Wenwei of the Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed, who led the research.
Significance of the study
The findings of the study have significant implications in cancer immunotherapy. Firstly, γδ-T-Exos interacted with CD44+/high NPC CSCs in high efficacy. Therefore, γδ-T-Exos can supplement radiotherapy and enhance its therapeutic efficacy against NPC. Secondly, γδ-T-Exos has advantages over other exosome-based therapies in combination with ionizing irradiation in NPC therapy (e.g. MSC-Exos) by preserving anti-tumor activities in the immunosuppressive NPC microenvironment and are easier in preparation. Thirdly, the results that γδ-T-Exos expanded pre-existing tumor-specific T cells in the immunosuppressive NPC microenvironment can greatly enhance the clinical feasibility of γδ-T-Exos. Therefore, it is important for the combination therapy to possess immunostimulatory effects to boost anti-tumor immunity in the immunosuppressive NPC microenvironment.

The research was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed. Credit: The University of Hong Kong
About the research team
The research was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed. Dr. Wang Xiwei, post-doctoral fellow of Professor Tu’s team, is the first author. Other researchers include Ms. Zhang Yanmei, PhD student; Dr. Mu Xiaofeng, post-doctoral fellow and Ms. Chung Yuet, Research Assistant of Professor Tu’s team; Ms. Chloe Tu Ran, Computational and Systems Biology Interdepartmental Program, University of California, Los Angeles, California, the United States. Professor George Tsao Sai-wah, Principal Lecturer, School of Biomedical Sciences, HKUMed. Professor Godfrey Chan Chi-fung, Tsao Yen-Chow Professor in Paediatrics and Adolescent Medicine, Clinical Professor of Paediatrics and Adolescent Medicine, HKUMed; Professor Leung Wing-hang, Chairperson and Clinical Professor, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed; Professor Lau Yu-lung, Doris Zimmern Professor in Community Child Health and Chair Professor of Paediatrics, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed; Dr. Liu Yinping, Research Officer, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed.
The Institute of Computational and Systems Biology Interdepartmental Program, University of California, Los Angeles, California, USA also contributed to this research.
Acknowledgments
This work was supported in part by Health and Medical Research Fund, Food and Health Bureau, Hong Kong SAR Government (18192021); Strategic Interdisciplinary Research Scheme, University of Hong Kong; General Research Fund (17122519, 17126317, 17114818, 17122420 and 17104617) from Research Grants Council, University Grants Committee, Government of the Hong Kong Special Administrative Region.
Reference: “Exosomes derived from γδ-T cells synergize with radiotherapy and preserve antitumor activities against nasopharyngeal carcinoma in immunosuppressive microenvironment” by Xiwei Wang, Yanmei Zhang, Xiaofeng Mu, Chloe Ran Tu, Yuet Chung, Sai Wah Tsao, Godfrey Chi-Fung Chan, Wing-Hang Leung, Yu-lung Lau, Yinping Liu and Wenwei Tu, February 2022, Journal for Immunotherapy of Cancer.
DOI: 10.1136/jitc-2021-003832







Be the first to comment on "A New Way To Stop Cancer: Researchers Combine Radiotherapy With Exosomes"