
Heavy alcohol consumption alters brain signaling pathways, impacting cognitive functions and promoting further drinking. Research in the journal Brain, Behavior and Immunity reveals that alcohol-dependent mice had increased levels of the immune signaling molecule IL-1β, which led to inflammation and altered neurotransmitter release. This finding could pave the way for improved treatments for alcohol use disorder by targeting the IL-1β pathway.
Heavy alcohol consumption creates a vicious cycle by altering signaling pathways in the brain, affecting cognitive functions and increasing the likelihood of further drinking. A study published in the journal Brain, Behavior and Immunity suggests that the brain’s immune system might be involved in this process. Alcohol-dependent mice showed twice as many cells producing the immune signaling molecule IL-1β in the medial prefrontal cortex, which regulates cognitive function. In these mice, IL-1β increased inflammation and release of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), persisting even after alcohol consumption ceased. This research may lead to improved treatment for alcohol use disorder (AUD) by targeting specific components of the IL-1β pathway.
Heavy alcohol use creates a vicious cycle: It changes signaling pathways in the brain, which in turn affects cognitive functions like decision-making and impulse control — and makes the individual more likely to drink.
The mechanism behind this may involve the brain’s immune system, according to a recent article in the journal Brain, Behavior and Immunity. Assistant Professor of Psychology Florence Varodayan, part of Binghamton University, State University of New York’s Developmental Alcohol Exposure Research Center, is the lead author of “Chronic ethanol induces a pro-inflammatory switch in interleukin 1ß regulation of GABAergic signaling in the medial prefrontal cortex of male mice.”
Varodayan began the project while she was a postdoctoral fellow in the lab of senior author Marisa Roberto, the Schimmel Family Chair of Molecular Medicine at The Scripps Research Institute. Other collaborators on the project include Binghamton University Assistant Professor of Pharmaceutical Sciences Tony Davis, as well as scientists in the Roberto lab, and at the University of California at San Diego, Louisiana State University Health Sciences Center, University of Texas at Austin and La Jolla Institute for Immunology.
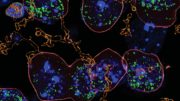
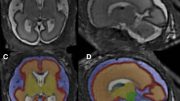
Compared to mice with moderate or no alcohol consumption, alcohol-dependent mice had twice as many cells producing the immune signaling molecule (IL-1ß) in their medial prefrontal cortex, a part of the brain that plays a role in regulating cognitive function. And the molecule’s pathway worked differently: Rather than its usual protective role, in alcohol-dependent mice IL-1ß increased inflammation and increased release of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA), which regulates neural activity in the brain. These changes persisted even when the mice no longer consumed alcohol.
“We suspected that IL-1ß was playing a role in AUD, but the exact mechanisms in the brain have been unclear,” Varodayan said.
Alcohol and the neuroimmune system
The molecule’s link to alcohol use disorder (AUD) was first uncovered by previous research; individuals with certain mutations in the gene that codes for IL-1ß are more prone to developing heavy levels of alcohol drinking, for example. Autopsies of people who suffered from AUD during life also showed higher levels of IL-1ß in the brain.
You can think of the neuroimmune system as a specialized immune system just for the brain, Varodayan explained. Just like our peripheral immune system, it works to eliminate pathogens and promote proper healing after injury. In addition to those features, it also plays a role in healthy brain function.
Researchers have discovered that alcohol “mildly” activates the neuroimmune system, meaning that the activation pattern is weaker than that caused by a pathogen or an injury. But changes from this mild activation seem to persist and accumulate over time as an individual drinks more heavily and more often, she said.
Here’s how it works: When the neuroimmune system responds to a pathogen or injury, it first releases neuroimmune factor IL-1ß, which triggers a quick, transient inflammatory response. This response is intended to resolve the injury or eliminate the pathogen, she explained. The neuroimmune system releases a second wave of anti-inflammatory factors to promote healing of affected brain cells.
“So, in the healthy brain, the neuroimmune system will resolve the ‘mild’ problem and the neurons will return to a healthy state. In the chronic ethanol brain, there will be ongoing inflammation that is likely an exaggerated response to the size of the initial problem,” she said. “This will likely lead to more widespread neuron damage that isn’t recoverable.”
Scientists hypothesize that the effects of heavy alcohol on neuroimmune signaling are linked to the cognitive decline seen in individuals with AUD. This research could potentially lead to improved treatment for substance abuse. Drugs that block the activity of IL-1ß are already approved by the U.S. Food and Drug Administration to treat rheumatoid arthritis and other inflammatory conditions.
“We plan to follow up on this study with more work on exactly how targeting specific components of the IL-1ß pathway might be useful in treating alcohol use disorder,” Roberto said.
Reference: “Chronic ethanol induces a pro-inflammatory switch in interleukin-1ß regulation of GABAergic signaling in the medial prefrontal cortex of male mice” by F.P. Varodayan, A.R. Pahng, T.D. Davis, P. Gandhi, M. Bajo, M.Q. Steinman, W.B. Kiosses, Y.A. Blednov, M.D. Burkart, S. Edwards, A.J. Roberts and M. Roberto, 28 February 2023, Brain, Behavior and Immunity.
DOI: 10.1016/j.bbi.2023.02.020






My Personal Alcohol Addiction Program (PAAP):
1) Buy donuts.
2) Take them to an AA meeting.
3) Sit there and listen.
I suggest scientists try making a drug to stop cigarettes. Faster results.