A single mutation allows SARS-CoV-2 to enter cells through a route that doesn’t rely on ACE2. While the ability to use an alternative entry pathway raises concerns about evading COVID-19 antibodies or vaccines, researchers did not find evidence of such evasion.
COVID-19 drugs, vaccines still effective against mutating virus.
Early in the COVID-19 pandemic, scientists identified how SARS-CoV-2, the virus that causes COVID-19, gets inside cells to cause infection. All current COVID-19 vaccines and antibody-based therapeutics were designed to disrupt this route into cells, which requires a receptor called ACE2.
Now, researchers at Washington University School of Medicine in St. Louis have found that a single mutation gives SARS-CoV-2 the ability to enter cells through another route – one that does not require ACE2. The ability to use an alternative entry pathway opens up the possibility of evading COVID-19 antibodies or vaccines, but the researchers did not find evidence of such evasion. However, the discovery does show that the virus can change in unexpected ways and find new ways to cause infection. The study is published June 23 in Cell Reports.
“This mutation occurred at one of the spots that changes a lot as the virus circulates in the human population,” said co-senior author Sebla Kutluay, PhD, an assistant professor of molecular microbiology. “Most of the time, alternative receptors and attachment factors simply enhance ACE2-dependent entry. But in this case, we have discovered an alternative way to infect a key cell type — a human lung cell — and that the virus acquired this ability via a mutation that we know arises in the population. This is something we definitely need to know more about.”
The finding was serendipitous. Last year, Kutluay and co-senior author M. Ben Major, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Cell Biology & Physiology, planned to study the molecular changes that occur inside cells infected with SARS-CoV-2. Most researchers study SARS-CoV-2 in primate kidney cells because the virus grows well in them, but Kutluay and Major felt it was important to do the study in lung or other cells similar to the ones that are naturally infected. To find more relevant cells capable of growing SARS-CoV-2, Kutluay and Major screened a panel of 10 lung and head-and-neck cell lines.
“The only one that was able to be infected was the one I had included as a negative control,” Major said. “It was a human lung cancer cell line with no detectable ACE2. So that was a crazy surprise.”
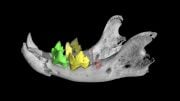
Kutluay, Major and colleagues — including co-first authors and postdoctoral researchers Maritza Puray-Chavez, PhD, and Kyle LaPak, PhD, as well as co-authors Dennis Goldfarb, PhD, an assistant professor of cell biology & physiology and of medicine, and Steven L. Brody, MD, the Dorothy R. and Hubert C. Moog Professor of Pulmonary Diseases in Medicine, and a professor of radiology — discovered that the virus they were using for experiments had picked up a mutation. The virus had originally been obtained from a person in Washington state with COVID-19, but as it was grown over time in the laboratory, it had acquired a mutation that led to a change of a single amino acid at position 484 in the virus’s spike protein. SARS-CoV-2 uses spike to attach to ACE2, and position 484 is a hot spot for mutations. A variety of mutations at the same position have been found in viral variants from people and mice, and in virus grown in the lab. Some of the mutations found in virus samples taken from people are identical to the one Kutluay and Major found in their variant. The Alpha and Beta variants of concern have mutations at position 484, although those mutations are different.
“This position is evolving over time within the human population and in the lab,” Major said. “Given our data and those of others, it is possible that the virus is under selective pressure to get into cells without using ACE2. In so many ways, it is scary to think of the world’s population fighting a virus that is diversifying the mechanisms by which it can infect cells.”
To determine whether the ability to use an alternative entry pathway allowed the virus to escape COVID-19 antibodies or vaccines, the researchers screened panels of antibodies and blood serum with antibodies from people who have been vaccinated for COVID-19 or recovered from COVID-19 infection. There was some variation, but in general, the antibodies and blood sera were effective against the virus with the mutation.
It is not yet clear whether the alternative pathway comes into play under real-world conditions when people are infected with SARS-CoV-2. Before the researchers can begin to address that question, they must find the alternative receptor that the virus is using to get into cells.
“It is possible that the virus uses ACE2 until it runs out of cells with ACE2, and then it switches over to using this alternative pathway,” Kutluay said. “This might have relevance in the body, but without knowing the receptor, we cannot say what the relevance is going to be.”
Major added, “That’s where we’re going right now. What is the receptor? If it’s not ACE2, what is it?”
Reference: “Systematic analysis of SARS-CoV-2 infection of an ACE2-negative human airway cell” by Maritza Puray-Chavez, Kyle M. LaPak, Travis P. Schrank, Jennifer L. Elliott, Dhaval P. Bhatt, Megan J. Agajanian, Ria Jasuja, Dana Q. Lawson, Keanu Davis, Paul W. Rothlauf, Zhuoming Liu, Heejoon Jo, Nakyung Lee, Kasyap Tenneti, Jenna E. Eschbach, Christian Shema Mugisha, Emily M. Cousins, Erica W. Cloer, Hung R. Vuong, Laura A. VanBlargan, Adam L. Bailey, Pavlo Gilchuk, James E. Crowe, Jr., Michael S. Diamond, D. Neil Hayes, Sean P.J. Whelan, Amjad Horani, Steven L. Brody, Dennis Goldfarb, M. Ben Major and Sebla B. Kutluay, Accepted, Cell Reports.
DOI: 10.1016/j.celrep.2021.109364
This work was supported in part by Washington University School of Medicine; V Foundation, grant number T2014-009; the National Institutes of Health (NIH), grant numbers T32CA009547-34, 5T32HL007106-39, K08HL150223, AI059371, AI157155, and 75N93019C00074; and the Defense Advanced Research Projects Agency, grant number HR001117S0019. This study utilized samples obtained from the Washington University School of Medicine’s COVID-19 biorepository supported by the NIH/National Center for Advancing Translational Sciences, grant number UL1 TR002345.






All the talk is about the spike proteins, but the real problem is in the virus and how coronaviruses may attack cells and why two of the most dangerous, MERS and Covid-19, are so infectious. My independent research has found multiple one-in-a-million nucleotide sequence matches between all the coronaviruses and the human genome. Those sequences are the same as some of the DHU loops of human tRNA. Using those loops and their anticodon matches, viruses may be able to fool the nucleus membrane in cells to allow the virus to enter and associate with the human DNA, creating more opportunities for further infection. Our immune system may be compromised and may no longer be able to stop the virus and other diseases from attacking organs throughout the body. Vaccines that attack the virus protein shells while ignoring their contents are doomed to failure from the Darwin effect, but recognizing these DHU loops suggests a possible approach to successful coronavirus vaccines. For MERS, eliminating the nucleotide sequence CAGTGGTAG from the virus may make it less infectious and stimulate the body to create antibodies to attack the entire virus. And eliminating the nucleotide sequence TAGTGGTGAG from Covid-19 may do the same thing. Only the infection process is considered in my work, not the innate virulence of the virus. For more info, check out this YouTube: https://www.youtube.com/watch?v=pd4OD4GpsJI
Yes, one of the accessory proteins is responsible for “silencing” the host cell, so it can’t call for help. That’s how the infection can spread before immune system can react. Ivermectin is one of the few drugs that can prevent this by blocking the viral mRNA. Patients who took Ivermectin showed up to 5000 times less spread of SARS-2, mainly because it could then be detected early and fought like a normal virus.
They are aware of the Neuropilin receptor and the gateway it uses to get to the brain using olfactory cells, right?
https://www.researchgate.net/publication/342005767_Neuropilin-1_facilitates_SARS-CoV-2_cell_entry_and_provides_a_possible_pathway_into_the_central_nervous_system