Researchers found that resistance to the leukemia drug venetoclax occurs due to increased breakdown and turnover of mitochondria in cancer cells, a process called mitophagy. They discovered that inhibiting mitophagy with chloroquine restores venetoclax’s ability to kill cancer cells, suggesting a potential future therapy for acute myeloid leukemia.
Future clinical trials will be conducted to investigate whether the combination of chloroquine and venetoclax can prevent disease recurrence.
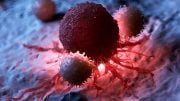
Although new drugs have been developed to induce cancer cell death in individuals with acute myeloid leukemia, the leukemic cells often develop resistance and evade the drugs’ effects within a year.
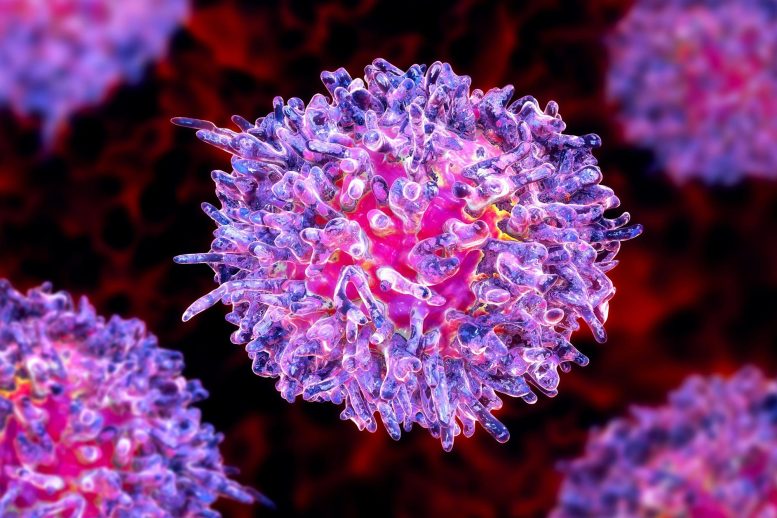
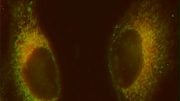
Recently, research conducted using both human tissue samples and mouse models has uncovered that the resistance of leukemia cells to the widely used drug venetoclax is due to an abrupt surge in the breakdown and turnover of mitochondria. These structures within the cell play a crucial role in generating energy and also signal the cell to undergo programmed cell death under certain adverse conditions.
This process of “programmed cell death” often goes wrong in cancer. Damaged mitochondria can also undergo a form of “self-eating” termed mitophagy that prevents them from sending “death signals.”
Led by scientists at NYU Langone Health and its Perlmutter Cancer Center, the study showed that mitophagy helps leukemia cells to evade the killing effects of venetoclax, a drug in a class of medications known as BH3 mimetics.
In a study recently published in the journal Cancer Discovery, researchers found that the levels of several genes associated with mitophagy were increased in 20 leukemia patient samples compared with normal controls. The level of these genes was even higher in samples from leukemia patients with drug resistance than in those leukemic patients who were not. Particularly notable was the increased expression of the gene for Mitofusin-2 (MFN2), which codes for a key protein in the outer mitochondrial membrane.
Further experiments using mice into which bone marrow from acute myeloid leukemia patients was transplanted showed that the drug chloroquine, a known mitophagy inhibitor, restored the ability of venetoclax to kill the cancer cells.
“Overcoming resistance to BH3 mimetic drugs like venetoclax is of unique clinical significance because these medications are often used for treating people with acute myeloid leukemia,” said study co-lead investigator Christina Glytsou, Ph.D., a former postdoctoral researcher at NYU Grossman School of Medicine and now an assistant professor at Rutgers University.
“Acute myeloid leukemia is notoriously difficult to treat, with fewer than a third of those affected living longer than five years after their diagnosis, so it is important to maximize the impact of existing therapies,” said study co-lead investigator Xufeng Chen, Ph.D., an instructor in the Department of Pathology at NYU Grossman.
“Our preclinical findings suggest that combining BH3 mimetics like venetoclax with either MFN2 or general mitophagy inhibitors could possibly serve as a future therapy for acute myeloid leukemia, as current drug treatments are stalled due to drug resistance,” said study senior investigator Iannis Aifantis, Ph.D.
Aifantis, the Hermann M. Biggs Professor and chair of the Department of Pathology at NYU Grossman and Perlmutter, says the research team plans to design a clinical trial to test whether chloroquine, when used in combination with venetoclax, prevents drug resistance in people with acute myeloid leukemia.
Speaking about other study results, the researchers say they not only found that MFN2 was overly active in people with drug-resistant disease, but also that cancer cells exposed to similar cell-death-inducing compounds demonstrated a doubling in mitophagy rates.
Additional testing in cancer cells engineered to lack MFN2 showed increased sensitivity to drugs similar to venetoclax compared with cells that had functional MFN2. The new study and previous research by the team showing misshapen mitochondria in drug-resistant leukemic cells confirmed that increased mitophagy was the source of the problem.
Acute myeloid leukemia, the most common form of adult leukemia, originates in the bone marrow cells and involves the rapid buildup of abnormal blood cells. The blood cancer results in the deaths of more than 11,500 Americans annually. Current treatments include chemotherapy and a limited number of targeted drug therapies. Bone marrow transplantation has also been used when other options fail.
Reference: “Mitophagy promotes resistance to BH3 mimetics in acute myeloid leukemia” by Christina Glytsou, Xufeng Chen, Emmanouil Zacharioudakis, Wafa Al-Santli, Hua Zhou, Bettina Nadorp, Soobeom Lee, Audrey Lasry, Zhengxi Sun, Dimitrios Papaioannou, Michael Cammer, Kun Wang, Tomasz Zal, Malgorzata Anna. Zal, Bing Z. Carter, Jo Ishizawa, Raoul Tibes, Aristotelis Tsirigos, Michael Andreeff, Evripidis Gavathiotis and Iannis Aifantis, 24 April 2023, Cancer Discovery.
DOI: 10.1158/2159-8290.CD-22-0601
The study was funded by the National Science Foundation. Additional funding support was provided by the Leukemia & Lymphoma Society and by AstraZeneca, which provided several of the BH3 mimetic drugs used in these experiments.
Aifantis has received additional research funding from AstraZeneca. This arrangement is being managed in accordance with the policies and practices of NYU Langone Health.




Be the first to comment on "Death to Blood Cancer Cells: New Drug Combination Could Revive the Power of Leading Treatment"