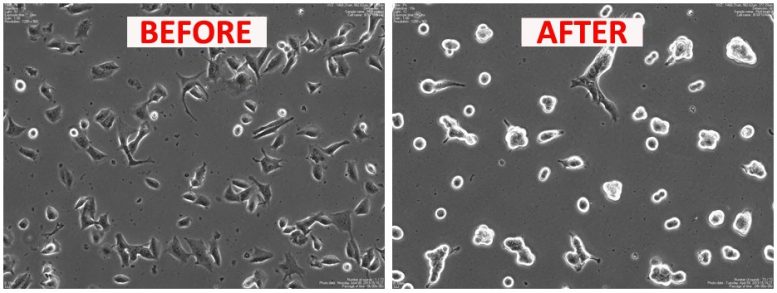
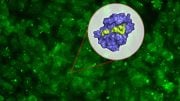
Cells treated with the experimental peptide Rb4 did not replicate and formed clusters, losing their natural morphology after just 24 hours of incubation.
Experimental treatment with a protein-derived molecule reduced tumor growth and metastasis as well as increased the survival rate by 25%
A recent study published in Scientific Reports demonstrates the effectiveness of Rb4, a peptide developed by Brazilian scientists, in combating cancer growth in an animal model, particularly malignant melanoma. The peptide also has the potential to treat drug-resistant tumors.
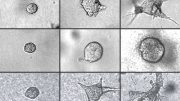
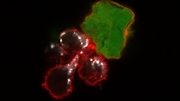
Rb4 causes necrosis in murine melanoma cells and decreases the viability of human cancer cells in preclinical in vitro and in vivo trials. Tumor cells in the experiment lost plasma membrane integrity, and mitochondria (energy-producing organelles) dilated even in the absence of chromatin condensation, a morphological hallmark of apoptosis. The researchers admit that they still don’t fully understand what causes this necrosis.
The peptide also reduced lung metastasis and decreased subcutaneous melanoma development in mice. The findings suggest that Rb4 acts directly on tumors, inducing the expression of two damage-associated molecular patterns (DAMPs) that cause immunogenic melanoma cell death.
“We do basic science in a search for novel molecules. In this study Rb4, which is derived from proteolipid protein 2 [PLP2], displayed a preference for causing necrosis, a specific type of cell death, especially in melanoma, but how this necrosis occurs and develops isn’t clear. The article discusses some aspects of the peptide’s morphological composition and the final effects of contact with it,” Fabrício Castro Machado, a co-author of the article, told Agência FAPESP.
Machado is a former member of the Department of Microbiology, Immunology and Parasitology’s Experimental Cancer Unit at the Federal University of São Paulo (UNIFESP) in Brazil, and is currently a researcher with Recepta Biopharma (ReceptaBio), a Brazilian biotech company that develops cancer drugs (hence the “Rb” in the peptide’s name).
With FAPESP’s support, a group led by Luiz Rodolpho Travassos, an emeritus professor at UNIFESP, began conducting the research. The authors of the article pay tribute to Travassos, who died in 2020. He published more than 230 articles in leading scientific journals, many of them on studies of peptides and peptidases (enzymes that break down proteins into peptides and eventually into single amino acids) in infectious diseases and cancer. Owing to this interest, in 2008 he contacted ReceptaBio, whose CEO is José Fernando Perez, a former Scientific Director of FAPESP (1993-2005).
“Professor Travassos identified several sequences of bioactive peptides, small molecules based on antibodies developed by ReceptaBio. Rb4 was also identified during this process of searching for novel molecules, although it isn’t derived from antibodies. We have another, Rb9, which is at a more advanced research stage, with several publications and patents, but still at the preclinical stage,” said Alice Santana Morais, a research and development analyst at ReceptaBio and corresponding author of the article.
In 2016, the scientists described the structure of Rb9 and its action mechanism as an inhibitor of melanoma cells. A more recent article published in 2020 showed that Rb9 acts as an immunomodulator and can be used to control tumor progression.
“Whether in academia or in companies like ReceptaBio, we need to combine efforts to conduct research. We’re looking for partners to boost the drug development process, which is lengthy and painstaking and requires discussion, details, and an exchange of experiences,” Morais said.
Promising results
Novel cancer treatments developed in recent years include peptide-based chemotherapy. Peptides have received increasing attention not only because they can bind to the membranes of tumor cells, but also because they have low molecular weights, good cell tissue penetration, and low toxicity for normal tissue. They can be used as cell reagents, ligands, vaccines, and carriers of cytotoxic drugs in peptide-alone therapy or peptide-conjugated materials.
In the study on Rb4’s anti-tumor action, the group found that the peptide interfered with the morphology, replication, and association of B16F10-Nex2 melanoma cells cultured in the laboratory. In contrast with controls, cells treated with Rb4 did not replicate and formed clusters, losing their natural morphology after incubation for at most 24 hours.
In addition, Rb4 reduced the number of lung metastatic nodules in a syngeneic melanoma model (involving tumor tissues from mice with the same genetic makeup). This result was detected after melanoma cells were injected intravenously into the mice. They were given five intraperitoneal injections of the peptide (300 micrograms per animal) on alternate days, delaying tumor growth by up to 40 days.
The survival rate of mice treated with Rb4 was significantly greater than that of the controls, increasing group survival by more than 25% and up to 10 days.
Melanoma originates in cells that produce melanin, the pigment that gives color to the skin. It can appear in various parts of the body. Although skin cancer is the most common form of cancer in Brazil, accounting for about 30% of all cases, melanoma represents only 3% of malignant neoplasias. It is the most life-threatening, however, because of the high probability of spreading to other organs (metastasis).
Around 8,400 cases of melanoma occur each year in Brazil, according to estimates by the National Cancer Institute (INCA). The disease caused 1,978 deaths in 2019.
Reference: “PLP2-derived peptide Rb4 triggers PARP-1-mediated necrotic death in murine melanoma cells” by Vera S. C. Maia, Rodrigo Berzaghi, Denise C. Arruda, Fabrício C. Machado, Leticia L. Loureiro, Pollyana M. S. Melo, Alice S. Morais, Alexandre Budu and Luiz R. Travassos, 21 February 2022, Scientific Reports.
DOI: 10.1038/s41598-022-06429-8





Be the first to comment on "Experimental Treatment Increases Skin Cancer Survival Rate by 25%"