
New research found that MRI May lead to overdiagnosis of cancer in older women. Illustration by Patrick Lynch / Yale University
New research from Yale University details how magnetic resonance imaging (MRI) for many women undergoing breast cancer surgery might identify health problems that would not otherwise impact patients — or lead to “overdiagnosis.”
Published in the Journal of Clinical Oncology, the study examined whether preoperative MRI use would allow doctors to identify breast cancer in the opposite breast (the one not affected by the diagnosed cancer) earlier, and therefore reduce the likelihood of advanced diseases in the future.
The researchers found that nearly half of the additional breast cancers detected by the preoperative MRI were overdiagnosed, which means that many of the cancers not detected by MRI would not have become clinically evident over the subsequent five years.
“This overdiagnosis is associated with false positive findings, psychological stress, more cancer detection, and costs, but does not prevent advanced disease or improve health outcomes,” said lead author Dr. Shiyi Wang, assistant professor of chronic disease epidemiology at Yale School of Public Health and a faculty member in the Cancer Outcomes, Public Policy, and Effectiveness Research (COPPER) Center at Yale School of Medicine and Yale Cancer Center.
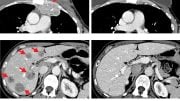
Wang and his colleagues analyzed the Surveillance, Epidemiology, and End Results-Medicare dataset. The team compared two groups of women who had breast cancer in terms of the occurrence of breast cancer in the opposite breast (i.e., contralateral breast cancer): One group had received an MRI, and another did not.
The team found that after five years, the MRI group had a higher incidence of cancer in the opposite breast than the non-MRI group (7.2% vs. 4.0%). “Specifically, MRI use would approximately double the detection rate of early-stage contralateral breast cancer, but would not decrease advanced-stage contralateral breast cancer occurrences after a five-year follow-up,” said Wang. “There was no evidence that MRI use was benefiting women because the rate of advanced cancer, whose prognosis is harmful, was similar in the MRI and the non-MRI groups.”
Dr. Cary Gross, senior author of the study and professor of internal medicine at Yale School of Medicine, said, “Patients and physicians need to balance the risks and benefits of preoperative MRI carefully. Preoperative breast MRI was associated with a large increase in detection rate of early-stage contralateral breast cancers, which led to additional treatments of the opposite breast.”
“This early detection by MRI use and the associated treatments would increase women’s suffering and stress, but did not prevent advance diseases or improve health outcomes,” added Gross, who is a member of Yale Cancer Center.
Other authors of the study include Jessica Long, Brigid Killelea, Suzanne Evans, Kenneth Roberts, and Andrea Silber.
This study was supported by a pilot grant and the P30 Cancer Center Support Grant (CCSG) at Yale Cancer Center.
Reference: “Preoperative Breast Magnetic Resonance Imaging and Contralateral Breast Cancer Occurrence Among Older Women With Breast Cancer” by Shi-Yi Wang, Jessica B. Long, Brigid K. Killelea, Suzanne B. Evans, Kenneth B. Roberts and Andrea SilberCary P. Gross, 30 November 2015, Journal of Clinical Oncology.
DOI: 10.1200/JCO.2015.62.9741




These researchers probably didn’t take in consideration the Lobular subtype of breast cancer, which is notoriously difficult to see in imaging and has a higher incidence of occurring in the opposite breast.
My breast surgeon advised me of the risk of over diagnosis from MRI. She and I chose to use the procedure anyway. I disagree with the quote from Dr Gross in the article – “This early detection by MRI use and the associated treatments would increase women’s suffering and stress, but did not prevent advance diseases or improve health outcomes,”. My MRI did, in fact, reveal previously undetected cancer on the opposite side. But my “suffering and stress” were not increased by the finding. Having chosen bilateral mastectomy, I am freed from the stress of repeated mammograms, and biopsies. I am pleased with the surgical outcome and would certainly not describe the result as “suffering”. For me, the more aggressive treatment was a suffering and stress REDUCER. We can not know whether my opposite side cancer would have ever become “advanced”, but if it had, a second immersion in testing, surgery, and other treatments would have been actual “suffering and stress”. Dr. Gross and all cancer specialists should not assume their patients are identical in their tolerance and reactions. Patients should be informed but must be allowed to choose.