
Tuberculosis is typically a disease of the lungs, but in the U.S. it can also be found in the bones in about 2 percent of cases.
Driving force behind strange tuberculosis outbreak was solved by a Duke collaboration.
Tuberculosis is most commonly associated with lung infections, however, in 2% of cases in the United States, it also affects the bones. This is a painful condition that leaves the bones looking like they’ve been gnawed. The 9,000-year-old skeletons of some Egyptian mummies exhibit telltale signs of having tuberculosis infection in their bones.
It was a weird puzzle when Duke physician Jason Stout M.D. encountered a peculiar Wake County, North Carolina tuberculosis outbreak in the mid-2000s in which the infection had spread beyond the lungs in six people. “Four out of six were in the bone,” Stout said. “That’s way more than 2 percent.”
The first person to have this strain of the disease in Raleigh, known as the index case, apparently contracted the bacterium while in Vietnam. He wasn’t feeling very sick and had been in contact with approximately 400 people in his workplace.
“So it was prolonged exposure in a workplace,” said Stout, a Duke professor of medicine who tracked down and identified seven subsequent infections through contact tracing and health department records.
All eight individuals were successfully treated with antibiotics and preventative care was given to their co-workers. Then the strange outbreak went away. However, the mystery was never really solved. “I’m an epidemiologist and clinical trial specialist and I was left scratching my head,” Stout said.
Until several years later when Stout had a chance conversation with his colleague and TB researcher David Tobin, Ph.D., an associate professor in molecular genetics and microbiology and immunology at Duke.
“We met up and we’re having coffee one day, and we’re talking about this,” Stout recalls. Academic medical centers like Duke routinely keep biological specimens, and Stout still had samples of the puzzling bug. “David said, ‘Well, give it to me and we’ll take a look.’ And then this amazing science came from that,” Stout said.
The amazing science is that Tobin’s lab, with several colleagues at Duke, Notre Dame, and the University of Texas, figured out precisely how and why these particular TB bacteria were so mobile. Their findings were published recently in the journal Cell.
“Certain infections tend to go certain places,” Stout said. “And the question is always, why does it do that?” In TB strains found in the Americas and Europe, the bacteria seem more likely to stay put in the lungs. But this strain was highly mobile.
Tobin’s team, led by Joseph Saelens, Mollie Sweeney, and Gopinath Viswanathan, ran genetic sequencing on the Raleigh bug and found it most resembled an ancestral strain from a group of strains called lineage 1. In the U.S. we tend to see the modern strains, lineages 2, 3, and 4, but lineage 1 is still out there, mostly in South and Southeast Asia.
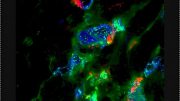
Mycobacterium tuberculosis generally infects a type of white blood cell called a macrophage, a highly mobile street sweeper cell that moves around looking for invaders and then engulfs them and chews them up. (Macrophage is Latin for big eater.) One part of the pathogenic bacteria’s toolkit is a set of unique chemical signals – secreted factors — to protect itself from the immune system and tell its macrophage host what to do.
Tobin’s team wanted to find the difference that allowed the Wake County bug’s macrophages to be more mobile and leave the lungs.
They compared genetic variants from 225 different strains of TB with particular attention to the genes for their secreted factors. What they found is a secretion factor called EsxM that was active in the Raleigh bacteria, but had been inactivated by a mutation in the modern strains.
Then, working with Craig Lowe, an evolutionary biologist and assistant professor of molecular genetics and microbiology at Duke, they looked at genetic sequencing from 3236 different strains of TB and found the pattern persisted: the modern strains have a silenced version of the EsxM secretion factor. “Over a few thousand strains, that really holds up,” Tobin said. “They’ve maintained that and presumably it’s something that’s evolutionarily advantageous to them.”
To further prove their point, the researchers put active versions of EsxM into safely attenuated versions of modern strains and watched as their macrophage hosts in a lab dish became more active and mobile. “We can see these changes in macrophage shape and structure and they become more migratory,” Tobin said. They also knocked out EsxM in a strain with the ancestral version and made the infected macrophages less mobile.
While being careful not to overstate their findings, Tobin said it would appear that the broadly distributed modern strains of TB benefit from staying within the lungs because of the way they spread through the air by breathing. Staying in the lungs would presumably give them a better launching pad to a new host.
Fortunately, the migratory TB strain hasn’t been seen again locally, Stout said, “hopefully because we did good work and got a lot of people preventative therapy.” But the mystery of its strange mobility has been solved.
“This may well have ended with me saying, ‘Wow, that was weird. There’s got to be something about the strain because all these patients had healthy immune systems,’” Stout said. “But the kind of science that I do is not the kind of science that David does. This is a wonderful example of people from different disciplines coming together to answer a really interesting clinical problem.”
Reference: “An Ancestral Mycobacterial Effector Promotes Dissemination of Infection” by Joseph W. Saelens, Mollie I. Sweeney, Gopinath Viswanathan, Ana María Xet-Mull, Kristen L. Juric Smith, Dana M. Sisk, Daniel D. Hu, Rachel M. Cronin, Erika J. Hughes, W. Jared Brewer, Jörn Coers, Matthew M. Champion, Patricia A. Champion, Craig B. Lowe, Claire M. Smith, Sunhee Lee, Jason E. Stout and David M. Tobin, 9 November 2022, Cell.
DOI: 10.1016/j.cell.2022.10.019
This research was supported by the National Institutes of Health (AI-125517, AI-130236, AI-127115, AI-142127, AI-149147, AI-106872, 1DP2-GM146458-01, UC6-AI-058607).






I worked at California TB Control many years ago. TB is a fascinating disease and often difficult to treat (mainly due to the population that is infected.) The US requires tests and/or x-rays to show an immigrant is TB free. Note: lung x-rays. Immigrants were sometimes caught with other people’s TB free x-rays; once a man presented a woman’s x-rays. There’s a whole industry of fake x-rays in foreign countries. Lucky us.
Aspertame and Garlic
Titanium oxide
In 1963 I had tb in my leg between my thigh and knee not in the bone,but I did not have it in the lungs . I spent 1yr in hospital but the medication did not work and the only way to get rid of it was by surgery. How was it possible for it to be in the leg and not in the lungs?
Parrot TB infecting humans.
In the 80s/90s, people interested in
buying imported parrots werevtold this story: baby parrots were caught and fed by local people who chewed good then fed that to the babies. The
Parrots then developed TB that passed to buyers of pet parrot. My bird was necropsied at nearby Vet Med School
which verified TB. Is the origin of TB in the US still coming from now illegal pet trade animals?
I have had this terrible pain in my chest area after surgery that stays in my bones and travels back and forth through my chest cavity front and back very painful. Dr.s don’t know and can’t explain it. Is there a blood test that will show this? Could this be that bone eating TB?
Is TB an axial type bacteria? Either way did anyone consider the fact that the antibiotics are what caused the bacteria to burrow into the bones because antibiotics cannot get them there.
To further my theory, the symptoms seems to get better with antibiotics but what actually happens is the symptoms change and get worse. Only blood test is if they look under a microscope but problem is they have to know what they are looking for and almost never do. Everything is too standardized for doctors to actually be helpful. Be your own advocate. If you can do your labs at a university instead of a hospital , go that route. They actually listen to you and try to help.