
Researchers from Brigham and Women’s Hospital found that step and time-based exercise goals are equally effective in reducing mortality and cardiovascular risk, suggesting that personal preference should guide the choice of physical activity targets. The study calls for future guidelines to incorporate flexible, inclusive measures of physical fitness.
According to new research, setting exercise goals based on steps or time is equally beneficial for health, suggesting that personal preference should guide the choice of exercise metrics.
Since the emergence of smartwatches, step-based exercise goals have become increasingly popular. However, current physical activity guidelines lack specific recommendations for step counts. In a new study, researchers from Brigham and Women’s Hospital have found that step-based and time-based exercise targets are equally effective at reducing the risk of premature death and cardiovascular disease. These findings, published on May 20 in JAMA Internal Medicine, suggest that the choice of a time-based exercise goal or a step-based one is largely a matter of personal preference.
The Current State of Exercise Guidelines
According to the current U.S. health guidelines, last updated in 2018, adults should engage in at least 150 minutes of moderate to vigorous physical activity per week, such as brisk walking, or 75 minutes of vigorous activities like jogging. Historically, these guidelines were based on self-reported physical activity data, with limited information on the health impacts of specific step counts. With the rise of wearable technology, step counts have become a popular exercise metric, prompting researchers to compare the benefits of time-based goals against step-based goals.
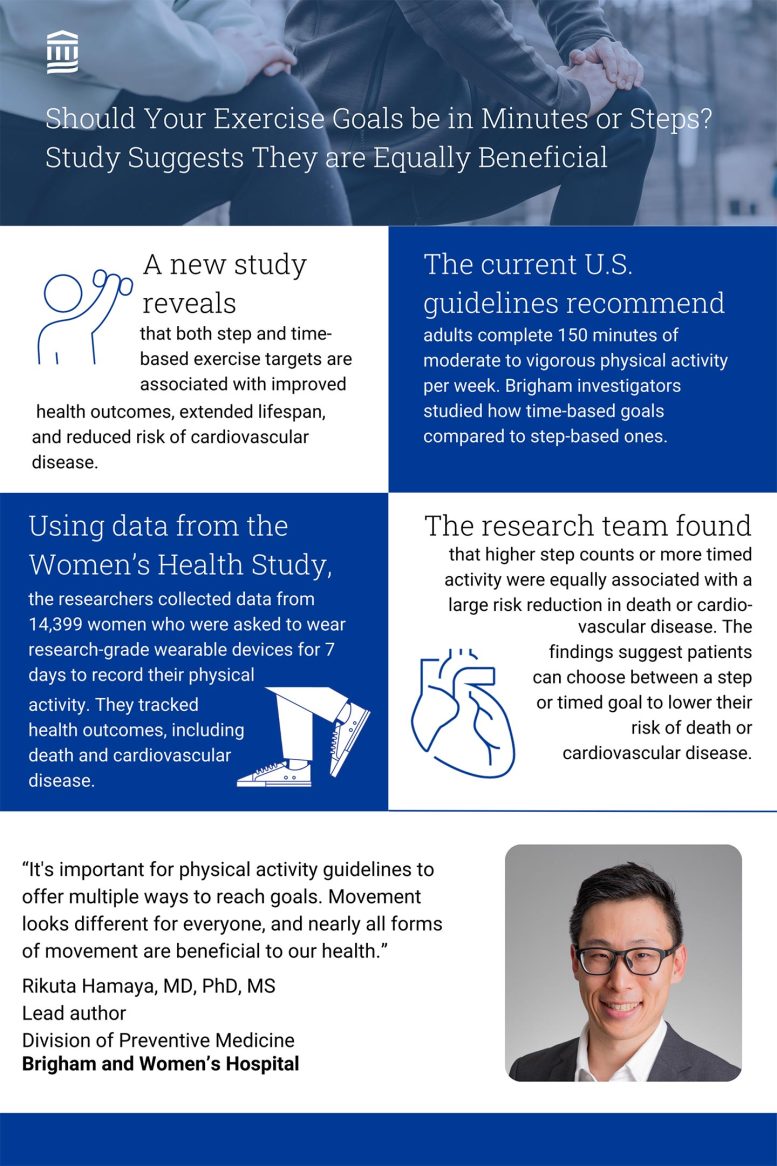
New research from Brigham and Women’s Hospital researchers reveals that both step and time-based exercise targets are equivalently associated with improved health outcomes, extended lifespan, and reduced risk of cardiovascular disease. Credit: Brigham and Women’s Hospital
Study Details and Findings
“We recognized that existing physical activity guidelines focus primarily on activity duration and intensity but lack step-based recommendations,” said lead author Rikuta Hamaya, MD, PhD, MS, a researcher in the Division of Preventive Medicine at BWH. “With more people using smartwatches to measure their steps and overall health, we saw the importance of ascertaining how step-based measurements compare to time-based targets in their association with health outcomes – is one better than the other?”
In this study, the researchers collected data from 14,399 women who participated in the Women’s Health Study and were free from cardiovascular disease and cancer. Between 2011 and 2015, participants aged 62 years and older were asked to wear research-grade wearables for seven consecutive days to record their physical activity levels, only removing the devices for sleep or water-related activities. Throughout the study period, annual questionnaires were administered to ascertain health outcomes of interest, in particular, death from any cause and cardiovascular disease. Investigators followed up with participants through the end of 2022.
At the time of device wear, researchers found that participants engaged in a median of 62 minutes of moderate-to-vigorous intensity physical activity per week and accumulated a median of 5,183 steps per day. During a median follow-up of 9 years, approximately 9% of participants had passed and roughly 4% developed cardiovascular disease.
Higher levels of physical activity (whether assessed as step counts or time in moderate-to-vigorous activity) were associated with large risk reductions in death or cardiovascular disease – the most active quarter of women had 30-40% risk reductions compared with the least active quarter. And, individuals in the top three quartiles of physical activity outlived those in the bottom quartile by an average of 2.22 and 2.36 months respectively, based on time and step-based measurements, at nine years of follow-up. This survival advantage persisted regardless of differences in body mass index (BMI).
Advantages and Limitations of Step Counting
While both metrics are useful in portraying health status, Hamaya explained that each has its advantages and downsides. For one, step counts may not account for differences in fitness levels. For example, if a 20-year-old and 80-year-old both walk for 30 minutes at moderate intensity, their step counts may differ significantly. Conversely, steps are straightforward to measure and less subject to interpretation compared to exercise intensity. Additionally, steps capture even sporadic movements of everyday life, not just exercise, and these kinds of daily life activities likely are those carried out by older individuals.
“For some, especially for younger individuals, exercise may involve activities like tennis, soccer, walking, or jogging, all of which can be easily tracked with steps. However, for others, it may consist of bike rides or swimming, where monitoring the duration of exercise is simpler. That’s why it’s important for physical activity guidelines to offer multiple ways to reach goals. Movement looks different for everyone, and nearly all forms of movement are beneficial to our health,” said Hamaya.
Implications for Future Guidelines
The authors note that this study incorporates only a single assessment of time and step-based physical activity metrics. Further, most women included in the study were white and of higher socioeconomic status. Finally, this study was observational, and thus causal relations cannot be proven. In the future, Hamaya aims to collect more data via a randomized controlled trial to better understand the relationship between time and step-based exercise metrics and health.
Senior author I-Min Lee, MBBS, ScD, an epidemiologist in the Division of Preventive Medicine at BWH, concluded, “The next federal physical activity guidelines are planned for 2028. Our findings further establish the importance of adding step-based targets, in order to accommodate flexibility of goals that work for individuals with differing preferences, abilities and lifestyles.”
Reference: “Time- vs Step-Based Physical Activity Metrics for Health” by Rikuta Hamaya, Eric J. Shiroma, Christopher C. Moore, Julie E. Buring, Kelly R. Evenson and I-Min Lee, 20 May 2024, JAMA Internal Medicine.
DOI: 10.1001/jamainternmed.2024.0892
Additional authors include Julie E. Buring and I-Min Lee, Eric Shiroma, Christopher Moore, and Kelly Evenson.
This research was supported in part by the National Institutes of Health (CA154647, CA047988, CA182913, HL043851, HL080467, and HL09935), from the; National Cancer Institute (5R01CA227122), Office of the Director, Office of Disease Prevention, and Office of Behavioral and Social Sciences Research; and by the extramural research program at the National Heart, Lung, and Blood Institute.








Be the first to comment on "You Don’t Have To Measure Minutes – New Study Challenges Traditional Exercise Guidelines"