
CNIO researchers have discovered that cells signaled to have excess nutrients can lead to organ malfunction and inflammation, potentially accelerating aging. Using animal models and comparisons with human blood samples, they have shown that targeting inflammation could mitigate aging symptoms and extend life, with implications for understanding diseases related to aging and obesity.
Researchers find that excess nutrients in cells trigger inflammation and organ dysfunction, accelerating aging. Their study suggests that interventions in inflammation might improve lifespan.
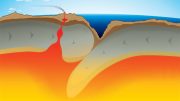
The accelerated aging of our population underscores the urgency to understand the molecular changes occurring in the body over time. The mTOR protein complex plays a critical role in many body functions, particularly in metabolism. A new study by Spanish National Cancer Research Center (CNIO) researchers shows that even slight increases in mTOR activity can induce premature aging in animal models, reducing their lifespan by up to 20%.
This study, published in Nature Aging, provides insights into why diseases associated with aging worsen in individuals with a high body mass index, an indicator of obesity and inflammation. It also explains why calorie restriction, known for extending lifespan in animals, promotes healthy aging by activating specific genes that interact with mTOR.
Additionally, the study introduces a new research tool designed “to study the relationship between nutrient increase and the ageing of different organs,” according to lead author Alejo Efeyan, who heads the Metabolism and Cell Signalling Group at the National Cancer Research Centre (CNIO).
Manipulating mTOR in Animal Models
The activity of the mTOR protein complex is regulated according to the amount of nutrients available in the cell. The authors developed a method to manipulate mTOR activity in animal models by targeting the protein that signals nutrient levels to mTOR. By genetically modifying this protein to simulate higher nutrient levels, they triggered mTOR to activate its pathway as if the animals were consuming more food, even though their actual diet remained unchanged.

Ana Ortega-Molina, primary author and current researcher at the Severo Ochoa Molecular Biology Centre, and Alejo Efeyan, senior author, from the CNIO Metabolism and Cell Signalling Group. Credit: Antonio Tabernero /CNIO
Consequences of Enhanced mTOR Activity
When animals with the modified protein reach maturity, their cellular functions begin to deteriorate, leading to aging symptoms such as thinner skin and damage to organs like the pancreas, liver, and kidneys. Immune system cells come to repair them but are overwhelmed by the amount of damage. They accumulate and, instead of repairing, trigger inflammation that further increases problems in those organs.
This cycle of damage and ineffective repair shortens the animals’ lifespans by 20%, equivalent to about 16 years in humans.
Potential Therapeutic Measures
The researchers aimed to disrupt this cycle by inhibiting the immune response that causes inflammation. As a result, organ damage improved enough to gain what in humans would be a few years of life.
First author Ana Ortega-Molina, who runs the Metabolism in Cancer and Ageing Laboratory at CBM, notes that acting on chronic inflammation is “a potential therapeutic measure that controls deterioration of health.”
Potential Human Implications
When the CNIO group manipulated mTOR to simulate an excess of nutrients, the resulting changes mirrored those seen in natural aging. They compared their model to colonies of naturally aging mice, including both their own and those maintained by the National Institute on Aging (NIA).
For example, the activity of lysosomes, which are the organelles with which the cell removes and recycles its waste, is reduced in both naturally aged and genetically modified animals. “When there is an excess of nutrients it makes sense that the cell shuts down the recycling activity of lysosomes, because this recycling operates especially when there are no nutrients,” Efeyan says.
This decrease in lysosomal activity also occurs in human aging, as verified by the group from the University of Valencia when contrasting blood samples from young people and septuagenarians.
A New Tool
Beyond this paper, Efeyan believes that this new animal model offers “ample fertile ground to ask more questions about how nutrient increase, or their signalling, facilitates processes in the different organs that allow us to understand their ageing in particular. Or, for example, investigate the relationship with neurodegenerative diseases, because there is some inflammation in the central nervous system. It’s a tool that many more people can use.”
Additional co-authors include Rafael de Cabo of the National Institute on Aging (NIA) in Bethesda, USA, Consuelo Borrás and Daniel Monleón, from the University of Valencia, and María Casanova-Acebes, head of the Cancer Immunity group at CNIO.
Reference: “A mild increase in nutrient signaling to mTORC1 in mice leads to parenchymal damage, myeloid inflammation and shortened lifespan” by Ana Ortega-Molina, Cristina Lebrero-Fernández, Alba Sanz, Miguel Calvo-Rubio, Nerea Deleyto-Seldas, Lucía de Prado-Rivas, Ana Belén Plata-Gómez, Elena Fernández-Florido, Patricia González-García, Yurena Vivas-García, Elena Sánchez García, Osvaldo Graña-Castro, Nathan L. Price, Alejandra Aroca-Crevillén, Eduardo Caleiras, Daniel Monleón, Consuelo Borrás, María Casanova-Acebes, Rafael de Cabo and Alejo Efeyan, 7 June 2024, Nature Aging.
DOI: 10.1038/s43587-024-00635-x
This work has been funded by, among others, the Spanish Ministry for Science, Innovation and Universities, the Spanish Research Agency, the European Regional Development Fund, the Spanish Association Against Cancer Research Scientific Foundation, “la Caixa” Banking Foundation, Olivia Roddom Oncology Research Grant, Intramural Research Program at the NIA, National Institutes of Health. Yurena Vivas, one of the authors, is a beneficiary of a CNIO Friends contract funded by the Domingo Martinez Foundation.








For me, as a now eighty year old lay American male battling mostly mild externally imposed chronic disease for forty-three years and counting, this “cutting-edge” study is at least eighteen years behind the times. I first wrote the US FDA of my lay findings of connections between allergies, added MSG, chronic disease and obesity in October of 2005 (obviously, now, in-vain).
Since, I’ve learned more of the inflammation/xanthine oxidase/uric acid/free radicals/calcium deficiency/MSG crossing the blood brain barrier and metabolic syndrome link and shared it, updating as possible, with more than 4,000 professional others of various specialties, mostly with the same results. Am I the only one who finds and shares my findings freely? However, I still haven’t found-out whether mice inherit and/or acquire the same kind of food and food additive allergies that humans do? And, I doubt they season their food with MSG. And, too, I was reminded recently that my (Dr. Arthur F. Coca’s, by 1935) kind of allergy reactions might also be labeled as MCAS (Mast Cell Activation Syndrome).
Shame! To use a grotesque and contemptible image to represent fat persons. Fat people do not eat impolitely, nor gobble, nor stuff our faces, etc etc – as you imply.
Current science itself exploded the widely accepted fallacy that being fat is simple greed and negligence.
Do better.
Yes, indeed, an inappropriate image. More importantly, I think, is to recognize now epidemic obesity as a mere symptom of now multi-generational externally imposed root causes; medically undiagnosed food allergies (e.g., Dr. Arthur F. Coca, by 1935), officially (FDA in the US) approved food poisoning (e.g., soy (early 1970s), MSG (1980), HFCS and TBHQ (1972), minimally), allergy and food poisoning ignorant and incompetent doctors and excessive related/resultant medical errors.
The stock photo depicts processed bologna slices (bad for you). Adrenaline in animal death for human consumption (bad for you). They Know their being murdered. Lectins in plants (inflammatory) natural occurring poisons for their survival. I was the Art-director for “ACCENT” flavor enhancer, aka MSG. Sorry no-one warned me at the time. It didn’t mean I was consuming it. I had to make a living like anyone else. No study at the time. I’m a vegan, Limit my lectins (took 20 years to find out what a lectin was). Get a pressure cooker to limit foods and food reactions, that inflame your body.
Interesting suggestion, isore. But, if pressure cooking can make a real difference, then I wonder why is pasteurized cow’s milk one of (if not the) worst of my allergens and most cereals, potatoes, and beans safe for me? And, with some essential nutrients mostly available through animals which graze, are you sure you’re getting enough of what’s essential? Hopefully.