
A recent study conducted by Japanese researchers has revealed that the interaction of angiotensin II-AT1 and prostaglandin E2-EP1 systems, amplified by high salt intake, causes hypertension that leads to emotional and cognitive impairment, which involves changes to tau protein and other enzymes in the brain. These findings, which were reversed by antihypertensive medication and genetic modification, suggest new potential therapeutic targets for hypertension-induced dementia, which is particularly significant given the rising cost of dementia treatment in aging societies like Japan.
Researchers have pinpointed two essential physiological mechanisms that are involved in hypertension induced by high salt consumption and cognitive and emotional impairment.
Defined as a deterioration of cognitive functions such as thinking, remembering, and reasoning, dementia is highly common in Japan. As it stands, there is a distinct lack of satisfaction with the treatment of this condition, given the absence of any curative drug therapy. With an ever-increasing aging population worldwide, the urgency for the development of preventive measures and therapeutic drugs for dementia is escalating.
The connection between cognitive impairment and excessive intake of table salt, a staple in food seasoning, is well established. High salt (HS) consumption can also lead to hypertension. To avert negative health consequences, the World Health Organization advocates for a restriction on salt consumption to under 5 g daily.
The involvement of angiotensin II (Ang II)—a hormone that plays a key role in regulating blood pressure and fluid balance—and its receptor “AT1”, as well as that of the physiologically important lipid molecule prostaglandin E2 (PGE2 and its receptor “EP1” in hypertension and neurotoxicity is well-recognized. However, the involvement of these systems in HS-mediated hypertension and emotional/cognitive impairment remains elusive.
To this end, a recent study published in the British Journal of Pharmacology thoroughly evaluated the aspects of HS-mediated hypertension and emotional/cognitive impairment. The study was performed by a team of collaborating researchers from Japan, and has shown how hypertension, mediated by the crosstalk between Ang II-AT1 and PGE2-EP1 causes emotional and cognitive dysfunction.
Author Hisayoshi Kubota from Fujita Health University’s Graduate School of Health Science comments, “Excessive salt intake is considered a risk factor for hypertension, cognitive dysfunction, and dementia. However, studies focusing on the interaction between the peripheral and central nervous system have not sufficiently investigated this association.”
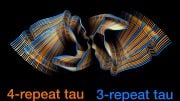
According to the published data, the addition of excessive phosphates to the protein “tau” is primarily responsible for these emotional and cognitive consequences. The findings are particularly noteworthy because tau is a key protein of Alzheimer’s disease.
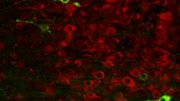
The team first loaded laboratory mice with an HS solution (2% NaCl in drinking water) for 12 weeks and monitored their blood pressure. “The effects of HS intake on emotional/cognitive function and tau phosphorylation were also examined in two key areas of the mouse brain—the prefrontal cortex and the hippocampus,” explains Prof. Mouri. Next, they also studied the involvement of the Ang II-AT1 and PGE2-EP1 systems in HS-induced hypertension and neuronal/behavioral impairment.
The results were remarkable and encouraging: The brains of the experimental mice had several biochemical alternations. At the molecular level, besides the addition of phosphates to tau, the researchers also observed a decrease in the phosphate groups linked to a key enzyme called “CaMKII”—a protein involved in brain signaling. Moreover, changes in the levels of “PSD95”—a protein that plays a vital role in the organization and function of brain synapses (the connection between brain cells)—were also evident. Interestingly, the biochemical changes were reversed after the administration of the antihypertensive drug “losartan.” A similar reversal was observed after knocking out the EP1 gene.
Overall, these findings suggest that angiotensin II-AT1 and prostaglandin E2-EP1 systems could be novel therapeutic targets for hypertension-induced dementia.
Prof. Mouri concludes by saying, “This study is of particular social and economic importance because the annual social cost of dementia treatment in Japan is surging like never before”. Therefore, developing preventive and therapeutic drugs for dementia seems critical for Japan’s rapidly aging population.”
Reference: “High salt induces cognitive impairment via the interaction of the angiotensin II-AT1 and prostaglandin E2-EP1 systems” by Hisayoshi Kubota, Kazuo Kunisawa, Bolati Wulaer, Masaya Hasegawa, Hitomi Kurahashi, Takatoshi Sakata, Hiroyuki Tezuka, Masanori Kugita, Shizuko Nagao, Taku Nagai, Tomoyuki Furuyashiki, Shuh Narumiya, Kuniaki Saito, Toshitaka Nabeshima and Akihiro Mouri, 19 April 2023, British Journal of Pharmacology.
DOI: 10.1111/bph.16093
The study was funded by the Japan Society for the Promotion of Science, the Japan Science and Technology Agency, Fujita Health University, the Smoking Research Foundation, and the Takeda Science Foundation.






Prevention beats cure. Switch from commercial table salt, pulluted with iodine and other chemicals, to the natural variety such as sea or Himalayan salt .