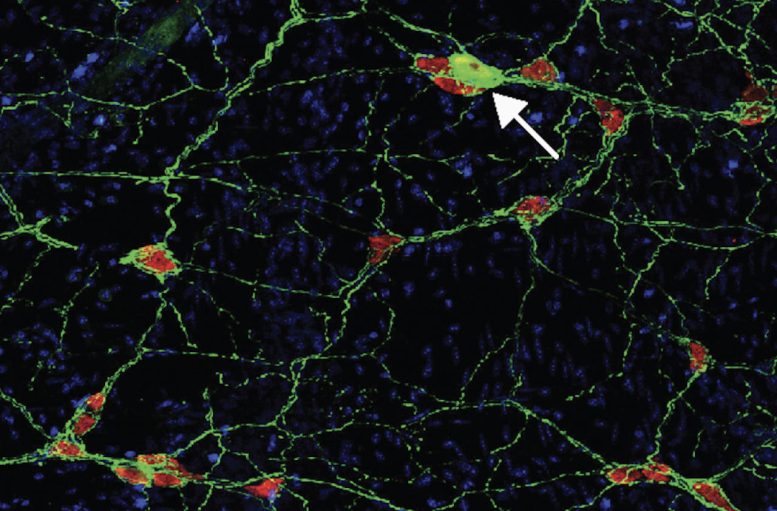
An autoimmune reaction in mice to a protein associated with Parkinson’s disease damaged neurons in the GI tract, adding to evidence that the disease may get its start in the gut. Credit: David Sulzer, Columbia University Irving Medical Center
Ask any neurologist and they’ll tell you: Parkinson’s disease is a disorder of the brain. The unmistakable signs of this ailment, such as involuntary shaking, reduced movement speed, and the sensation of one’s feet being glued to the floor, originate from the loss of neurons in a brain area responsible for movement regulation.
However, a growing number of scientists theorize that the roots of this neurodegenerative condition might be traced back to the gut, potentially manifesting long before any neurological symptoms emerge.
New findings by Columbia researchers David Sulzer, Ph.D., and Dritan Agalliu, Ph.D., and two of their graduate students are adding to evidence backing this hypothesis—and showing that what triggers initial gastrointestinal changes in Parkinson’s could be a misdirected immune attack.
“If this is the beginning of Parkinson’s in many people, we could potentially identify who has the disease before it ever reaches the brain and hopefully stop it in its tracks,” Sulzer says. The new findings were recently published in the journal Neuron.
Autoimmunity and the gut
The gut-first theory of Parkinson’s, originally proposed 20 years ago, started to intrigue Sulzer after his own research pointed toward the role of an autoimmune response in Parkinson’s.
In Parkinson’s, a protein called alpha-synuclein becomes misfolded, accumulates inside neurons, and slowly poisons the cells. Sulzer’s lab in collaboration with immunologists at the La Jolla Institute of Immunology has shown that small portions of the misfolded alpha-synuclein also can appear on the outside of neurons, which makes the neurons vulnerable to attack from the immune system. The immune attack could be doing more acute damage to the neurons than the internal deposits of alpha-synuclein.
“The blood of Parkinson’s patients often contains immune cells that are primed to attack the neurons,” Sulzer says, “but it’s not clear where or when they are primed.”
The gut was an intriguing possibility because it contains the same neurons and because most Parkinson’s patients experience constipation years before brain symptoms emerge and the disease is diagnosed. To pursue this hypothesis, Sulzer teamed up with Agalliu, a neuroimmunologist with expertise in mouse models of another neurological disorder (multiple sclerosis) that has autoimmune features.
Immune response to alpha-synuclein leads to gut symptoms
To find out if an immune reaction to alpha-synuclein can kick-start the disease and where, Francesca Garretti and Connor Monahan, grad students directed by Agalliu and Sulzer, first created a mouse capable of displaying pieces of misfolded alpha-synuclein on cell surfaces (natural mice do not have this ability). They then injected the mice with alpha-synuclein and monitored what happened in the brain and the gut.
The researchers did not see any signs resembling Parkinson’s disease in the brain, but they did see that an immune attack on neurons in the gut produced constipation and other gastrointestinal effects resembling those seen in most Parkinson’s patients years before they are diagnosed with the disease.
“This shows that an autoimmune reaction can lead to what appears to be the early stages of Parkinson’s and is strong support that Parkinson’s is in part an autoimmune disease,” Sulzer says.
The findings also raise the possibility that early detection—and then interruption—of an immune response in the gut could prevent a later attack on the brain’s neurons and stop Parkinson’s in its tracks.
Wanted: A mouse with Parkinson’s disease
Right now, though, it’s not clear how big a role the immune system plays in the Parkinson’s brain. The answer to that question may become clearer if the researchers find out why the brains of their mice did not develop any signs of Parkinson’s.
The team hypothesizes that the immune cells in their mouse model may not be reaching the brain because the animals are young and age has not yet weakened the blood-brain barrier sufficiently to let immune cells squeeze through. Opening the barrier or accelerating the aging process may lead to mice that develop gastrointestinal and brain symptoms.
“Our ultimate goal is to develop a model of Parkinson’s disease in mice that recreates the human disease process, which doesn’t exist right now,” Sulzer says. “That will be critical in answering questions about the disease that we can’t explore in people and eventually developing better therapies.”
Reference: “Interaction of an α-synuclein epitope with HLA-DRB1∗15:01 triggers enteric features in mice reminiscent of prodromal Parkinson’s disease” by Francesca Garretti, Connor Monahan, Nicholas Sloan, Jamie Bergen, Sanjid Shahriar, Seon Woo Kim, Alessandro Sette, Tyler Cutforth, Ellen Kanter, Dritan Agalliu and David Sulzer, 18 August 2023, Neuron.
DOI: 10.1016/j.neuron.2023.07.015
This research was funded by Aligning Science Across Parkinson’s through the Michael J. Fox Foundation for Parkinson’s Research, the National Institutes of Health; the JPB Foundation; the National MS Society, and gifts from Newport Equities LLC, the Walz family, and PANDAS Network to the Department of Neurology at Columbia University.







Be the first to comment on "Beyond the Brain: Unveiling the Unexpected Origins of Parkinson’s Disease"