
People who have had COVID-19 are at an elevated risk of developing neurological conditions within the first year after infection, according to a detailed analysis of federal data by researchers at Washington University School of Medicine in St. Louis. Movement disorders, memory problems, strokes, and seizures are among the complications. Credit: Sara Moser/Washington University School of Medicine
Strokes, seizures, memory, and movement disorders are among problems that develop in the first year after infection.
If you’ve had COVID-19, it may still be messing with your brain. According to new research, those who have been infected with the SARS-CoV-2 virus are at increased risk of developing a range of neurological conditions in the first year after the infection. A comprehensive analysis of federal health data reveals that such complications include strokes, cognitive and memory problems, anxiety, depression, and migraine headaches.
“Our study provides a comprehensive assessment of the long-term neurologic consequences of COVID-19.” — Ziyad Al-Aly, MD
In addition, the post-COVID brain is associated with movement disorders, from tremors and involuntary muscle contractions to epileptic seizures, balance and coordination difficulties, and hearing and vision abnormalities as well as other symptoms similar to what is experienced with Parkinson’s disease.
The findings, by researchers at Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care system, were published on September 22 in the journal Nature Medicine.
“Our study provides a comprehensive assessment of the long-term neurologic consequences of COVID-19,” said senior author Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University. “Past studies have examined a narrower set of neurological outcomes, mostly in hospitalized patients. We evaluated 44 brain and other neurologic disorders among both nonhospitalized and hospitalized patients, including those admitted to the intensive care unit. The results show the devastating long-term effects of COVID-19. These are part and parcel of long COVID. The virus is not always as benign as some people think it is.”
Al-Aly said that overall, COVID-19 has contributed to more than 40 million new cases of neurological disorders worldwide.
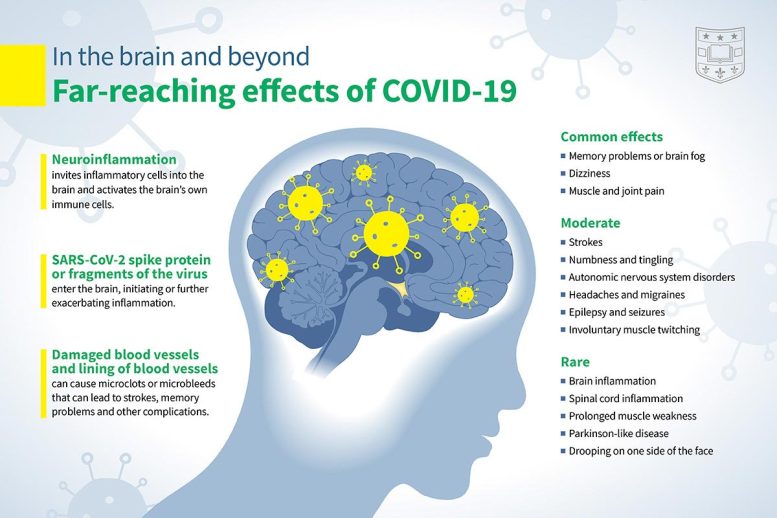
A comprehensive analysis of federal data by researchers at Washington University School of Medicine in St. Louis shows people who have had COVID-19 are at an elevated risk of developing neurological conditions within the first year after infection. Movement disorders, memory problems, strokes, and seizures are among the complications. Credit: Sara Moser/Washington University School of Medicine
Other than having a COVID-19 infection, specific risk factors for long-term neurological problems are lacking. “We’re seeing brain problems in previously healthy individuals and those who have had mild infections,” Al-Aly said. “It doesn’t matter if you are young or old, female or male, or what your race is. It doesn’t matter if you smoked or not, or if you had other unhealthy habits or conditions.”
Very few of the study participants were vaccinated for COVID-19. This is because the vaccines were not yet widely available during the time span of the study, which ran from March 2020 through early January 2021. Notably, the data also predates delta, omicron, and other COVID variants.
“Overall, COVID-19 has contributed to more than 40 million new cases of neurological disorders worldwide.”
A previous study led by Al-Aly that was published in Nature Medicine found that vaccines slightly reduce — by about 20% — the risk of long-term brain problems. “It is definitely important to get vaccinated but also important to understand that they do not offer complete protection against these long-term neurologic disorders,” Al-Aly said.
The scientists analyzed about 14 million de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs. They are the nation’s largest integrated healthcare system, and patients included all ages, races, and sexes.
Next, the research team created a controlled data set of 154,000 people who had tested positive for COVID-19 sometime from March 1, 2020, through January 15, 2021, and who had survived the first 30 days after infection. Neurological outcomes in the COVID-19 data set were compared using statistical modeling with two other groups of people not infected with the virus: a control group of more than 5.6 million patients who did not have COVID-19 during the same time frame; and a control group of more than 5.8 million people from March 2018 to December 31, 2019, before the pandemic which as left millions across the globe infected and killed by the SARS-CoV-2 virus.

Ziyad Al-Aly, MD, has led multiple studies on long COVID as a clinical epidemiologist at Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care system. His research has included the devastating effects of the virus on the heart, kidneys, and mental health. Credit: Matt Miller/Washington University School of Medicine
Brain health was analyzed by the scientists over a year-long period. Compared with those who had not been infected with the virus, neurological conditions were 7% more common in people with COVID-19. Extrapolating this percentage based on the number of COVID-19 cases in the U.S. translates to approximately 6.6 million people who have suffered brain impairments associated with the SARS-CoV-2 virus.
One of the most common brain-related, long-COVID symptoms is memory problems — colloquially called brain fog. People who contracted the virus were at a 77% increased risk of developing memory problems compared with those in the control groups. “These problems resolve in some people but persist in many others,” Al-Aly said. “At this point, the proportion of people who get better versus those with long-lasting problems is unknown.”
Interestingly, the research team noted an increased risk of Alzheimer’s disease among those infected with the virus. Compared with the control groups, there were two more cases of Alzheimer’s per 1,000 people with COVID-19. “It’s unlikely that someone who has had COVID-19 will just get Alzheimer’s out of the blue,” Al-Aly said. “Alzheimer’s takes years to manifest. But what we suspect is happening is that people who have a predisposition to Alzheimer’s may be pushed over the edge by COVID, meaning they’re on a faster track to develop the disease. It’s rare but concerning.”
Also, people who had the virus were 50% more likely to suffer from an ischemic stroke compared to the control groups. This is when a blood clot or other obstruction blocks an artery’s ability to supply blood and oxygen to the brain. Ischemic strokes account for the majority of all strokes, and can lead to difficulty speaking, vision problems, cognitive confusion, the loss of feeling on one side of the body, paralysis, permanent brain damage, and death.
“There have been several studies by other researchers that have shown, in mice and humans, that SARS-CoV-2 can attack the lining of the blood vessels and then trigger a stroke or seizure,” Al-Aly said. “It helps explain how someone with no risk factors could suddenly have a stroke.”
Overall, compared to the uninfected, people who had COVID-19 were 80% more likely to suffer from epilepsy or seizures, 43% more likely to develop mental health disorders such as anxiety or depression, and 35% more likely to experience mild to severe headaches. They were also 42% more likely to encounter movement disorders, which includes involuntary muscle contractions, tremors, and other Parkinson’s-like symptoms.
COVID-19 sufferers were also 30% more likely to have eye problems such as blurred vision, dryness, and retinal inflammation. They were also 22% more likely to develop hearing abnormalities such as tinnitus, or ringing in the ears.
“Our study adds to this growing body of evidence by providing a comprehensive account of the neurologic consequences of COVID-19 one year after infection,” Al-Aly said.
Long COVID’s effects on the brain and other systems emphasize the need for governments and health systems to develop policy, and public health and prevention strategies to manage the ongoing pandemic and devise plans for a post-COVID world, Al-Aly said. “Given the colossal scale of the pandemic, meeting these challenges requires urgent and coordinated — but, so far, absent — global, national, and regional response strategies,” he said.
Reference: “Long-term neurologic outcomes of COVID-19” by Evan Xu, Yan Xie and Ziyad Al-Aly, 22 September 2022, Nature Medicine.
DOI: 10.1038/s41591-022-02001-z
This research was funded by the U.S. Department of Veterans Affairs; the American Society of Nephrology; and KidneyCure. The data that support the findings of this study are available from the U.S. Department of Veterans Affairs. VA data are made freely available to researchers behind the VA firewall with an approved VA study protocol.







When humans use Crisper to f*@k with viruses and then that virus escapes into the human population, its just murder. Its all coming out now and someone needs to be hanged. Add to that, when Trump said operation warp speed on Vaccines…well now you see why I personally said f*@k off. Now people with poor luck are paying the Vaccine price. Stop following your leaders orders. They are self serving and do not care about you.
Yet another statistical modeling “study”. You can make it say whatever you want.
Not saying that getting covid is a good thing, but this seems to lump every and any “neurological” condition and blames it on covid. It’s been only 3 years with covid. You cannot make such sweeping conclusions for “long term” effects. So, the big question is: who is the money behind the study and what’s the motivation or agenda?
I must be one of the “lucky” ones.
Having had COVID twice I have had experienced ZERO side effects described here.
I’ve been having major tremors and shaking ever since I’ve had COVID. I don’t know if there’s any correlation, but I was fine before. My doctors think I have FND so I don’t know. It sucks.
Hey “cakitooka”:
statistics does not work that way. You can reject an test but you never accept one – only that you fail to reject it! When you think about it that way it gives the interpretation a lot of leeway!
G
Professor, didn’t you just agreed with what I said. You can make a statistical study do what you want for you based on what you reject (which is indirectly accepting the alternative), where you collect your data, how you massage the numbers, etc. That’s why we see repeated stories that one day coffee causes cancer and the next month it extends your life (just illustrative example. You can substitute anything else for “coffee”).
Starting with the FDA in October of 2005, I’ve been writing about undiagnosed food allergies aggravated with added ‘cultured-free’ MSG causing obesity, chronic diseases and premature mortality for almost seventeen years now. It’s just as likely misdiagnosis, mistreatment, vaccinations and/or medical errors are responsible for any new conditions presenting so early on. And, I’ve often wondered if they didn’t just create the Covid-19 ‘scamdemic’ to cover-up the ‘silent genocide’ of unsuspecting Americans just since 1980, the year added MSG was FDA approved for expanded use as an alleged ‘flavor-enhancer, as the word gets out.