In Denmark, advancements in artificial intelligence have significantly improved the detection of breast cancer while reducing false positives
In Denmark, AI has significantly improved breast cancer screening by increasing detection rates and reducing false positives, as found in a study published in the journal Radiology. AI reduced the workload of radiologists by classifying mammograms likely to be normal, thus decreasing the need for double readings and enhancing overall screening efficiency.
Breast radiologists in Denmark have enhanced the performance of breast cancer screenings and lowered the incidence of false-positive results using artificial intelligence (AI). Results of the study were published today (June 4) in Radiology, a journal of the Radiological Society of North America (RSNA).
While mammography successfully reduces breast cancer mortality, it also carries the risk of false-positive findings. In recent years, researchers have studied the use of AI systems in screening.
Potential of AI in Enhancing Screening
“We believe AI has the potential to improve screening performance,” said Andreas D. Lauritzen, Ph.D., a post-doctoral student at the University of Copenhagen and researcher at Gentofte Hospital in Denmark.
When used to triage likely normal screening results or assist with decision support, AI also can substantially reduce radiologist workload.
“Population-based screening with mammography reduces breast cancer mortality, but it places a substantial workload on radiologists who must read a large number of mammograms, the majority of which don’t warrant a recall of the patient,” Dr. Lauritzen said. “The reading workload is further compounded when screening programs employ double reading to improve cancer detection and decrease false-positive recalls.”
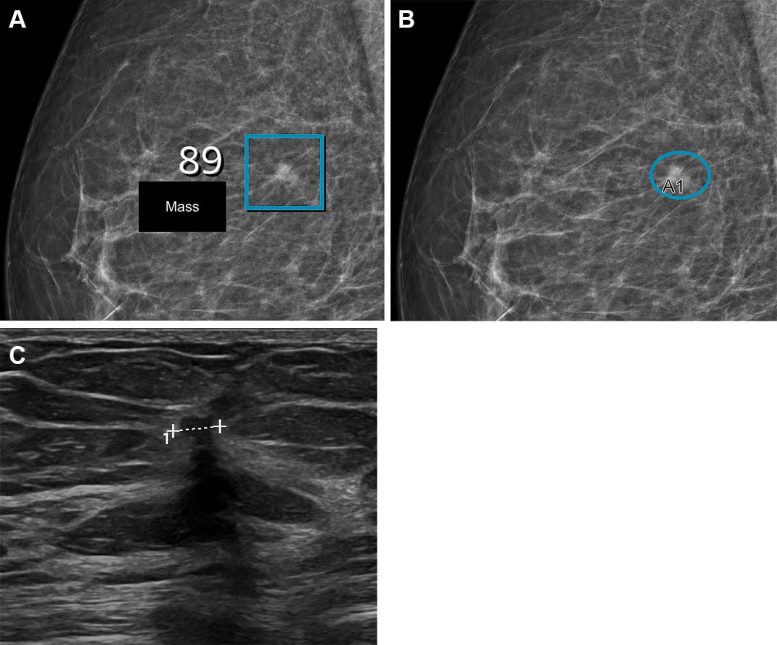
Images in a woman who had a Breast Imaging Reporting and Data System density of 2 and was 57 years old when she underwent screening with the artificial intelligence (AI) system. (A) Right mediolateral oblique full-field digital mammographic view shows AI-provided marking (square). The screening received a high AI examination score of 10 based on this lesion with a score of 89 out of 100. (B) Same image as in A, but with findings by the radiologists. Because of the high AI examination score, the screening was double read by two radiologists, who marked the same lesion (oval, A1) as the AI system, which led to recall. (C) Cropped US image shows a small (4 × 7 mm) invasive carcinoma (line) that was observed during the diagnostic workup. Credit: Radiological Society of North America (RSNA)
Study Design and Methods
Dr. Lauritzen and colleagues set out to compare workload and screening performance in two cohorts of women who underwent screening before and after AI implementation.
The retrospective study compared two groups of women between the ages of 50 and 69 who underwent biennial mammography screening in the Capital Region of Denmark.
In the first group, two radiologists read the mammograms of women screened between October 2020 and November 2021 before the implementation of AI. The screening mammograms of the second group of women performed between November 2021 and October 2022 were initially analyzed by AI. Mammograms deemed likely to be normal by AI were then read by one of 19 specialized full-time breast radiologists (called a single-read). The remaining mammograms were read by two radiologists (called a double-read) with AI-assisted decision support.
The commercially available AI system used for screening was trained by deep learning models to highlight and rate suspicious lesions and calcifications within mammograms. All women who underwent mammographic screening were followed for at least 180 days. Invasive cancers and ductal carcinoma in situ (DCIS) detected through screening were confirmed through needle biopsy or surgical specimens.
Results of AI Implementation
In total, 60,751 women were screened without AI, and 58,246 women were screened with the AI system. In the AI implementation group, 66.9% (38,977) of the screenings were single-read, and 33.1% (19,269) were double-read with AI assistance.
Compared to screening without AI, screening with the AI system detected significantly more breast cancers (0.82% versus 0.70%) and had a lower false-positive rate (1.63% versus 2.39%).
“In the AI-screened group, the recall rate decreased by 20.5 percent, and the radiologists’ reading workload was lowered by 33.4 percent,” Dr. Lauritzen said.
The positive predictive value of AI screening was also greater than that of screening without AI (33.5% versus 22.5%). In the AI group, a higher proportion of invasive cancers detected were 1 centimeter or less in size (44.93% vs. 36.60%).
Implications and Future Research
“All screening performance indicators improved except for the node-negative rate which showed no evidence of change,” Dr. Lauritzen said.
Dr. Lauritzen said more research is needed to evaluate long-term outcomes and ensure overdiagnosis does not increase.
“Radiologists typically have access to the women’s previous screening mammograms, but the AI system does not,” he said. “That’s something we’d like to work on in the future.”
It is also important to note that not all countries follow the same breast cancer screening protocols and intervals. U.S. breast cancer screening protocols differ from protocols used in Denmark.
Reference: “Early Indicators of the Impact of Using AI in Mammography Screening for Breast Cancer” by Andreas D. Lauritzen, Martin Lillholm, Elsebeth Lynge, Mads Nielsen, Nico Karssemeijer, Ilse Vejborg, 4 June 2024, Radiology.
DOI: 10.1148/radiol.232479
Collaborating with Dr. Lauritzen were Martin Lillholm, Ph.D., Elsebeth Lynge, Ph.D., Mads Nielsen, Ph.D., Nico Karssemeijer, Ph.D., and Ilse Vejborg, M.D.





Be the first to comment on "Fewer False Positives: AI Transforms Breast Cancer Screenings With Sharper Accuracy"